Composition of Urine
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Urinary System
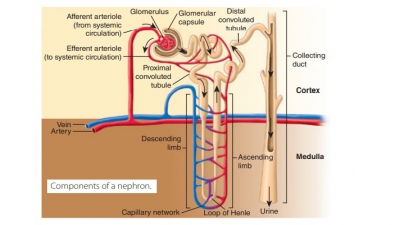
Urine is the final product of glomerular filtration, tubular reabsorption, and tubular secretion, and contains both filtered and secreted substances.
Composition
of Urine
Urine is the final product of glomerular filtration, tubular
reabsorption, and tubular secretion, and contains both filtered and secreted
substances. Every minute, about 1,200 mL of blood pass through the glomeruli.
Of this, 650 mL are plasma and, approxi-mately, 125 mL are filtrate forced into
the glomerular capsules. At this rate, the entire plasma volume is fil-tered
more than 60 times every day. Urea is a
result of amino acid catabolism and its plasma concentration reflects the
amount of protein in the diet. Urea fil-ters into the renal tubule with about
80% reabsorbed, whereas the remainder is excreted in the urine. Uric acid is
a result of metabolism of certain organic bases in nucleic acids. Active transport reabsorbs
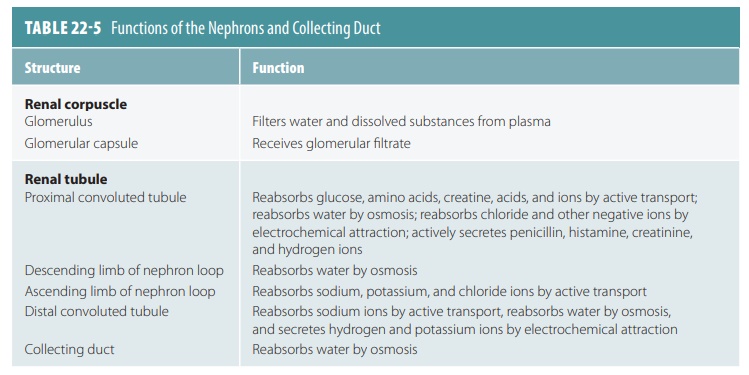
most of the uric acid present in the glomerular filtrate. TABLE 22-5 summarizes some
specific functions of the nephron segments and the collecting duct.
The chemical composition of urine is related to water volume
and the amount of solutes the kidneys must eliminate or retain to maintain
homeostasis. Urine is about 95% water, and usually contains urea and uric acid.
It may have traces of amino acids and electrolytes. Urine production varies
between 0.6 and 2.5 liters per day. Urine production of 50–60 mL per hour is
normal, with output of less than 30 mL per hour possibly indicating kidney
failure. In decreasing concentrations, urine contains mostly urea, followed by
sodium, potassium, phosphate, sulfate, creatinine, and uric acid. Tiny yet
variable amounts of calcium, magnesium, and bicarbonate are also present. The
analysis of urine samples is called urinalysis.
The physical characteristics of urine include color,
transparency, odor, pH, and specific gravity. When freshly voided, normal urine
is clear, with a color between pale and deep yellow. The color is caused by the
pigment urochrome, which
results from the destruction of hemoglobin. Higher concentrations cause the
urine to be deeper yellow. When fresh, urine is slightly aromatic, but after
standing for a while, it develops an odor of ammonia. This is because of
bac-teria that metabolize the urea solutes. Normally, urine is slightly acidic,
with a pH of 6. However, dietary or metabolic changes may cause its pH to
change, rang-ing from 4.5 to 8. The specific
gravity of urine is slightly higher than that of distilled water. This is
because of the solutes it contains. Normal urine specific gravity is between 1.001
and 1.035, whereas distilled water’s specific gravity is 1. Specific gravity is
defined as the ratio of the mass of a substance to the mass of an equal volume
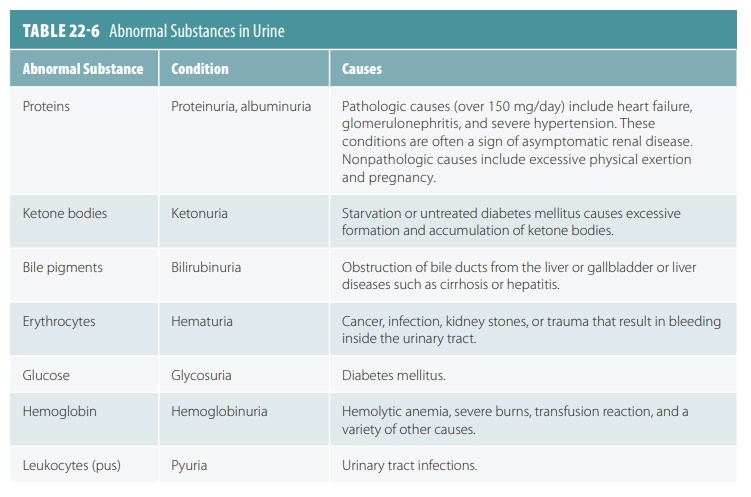
of distilled water. Abnormal substances in the urine are explained in TABLE 22-6.
Renal Clearance
The volume of plasma from which the kidneys com-pletely
remove a particular substance over a specific time period, usually one minute,
is known as renal clearance. Tests are performed to
determine the glomerular filtration rate. This allows detection of
glo-merular damage and renal disease. For any substance, the renal clearance
rate, abbreviated “C,” is calculated in milliliters per minute, using this
equation:
C = UV/P
where U is the
concentration of the substance in urine, calculated in milligrams per
milliliter; V is the flow rate of
urine formation, calculated in milliliters per minute; and P is the concentration of the substance in plasma, calculated in
milligrams per milliliter.
To determine the GFR, the substance used is inulin. This is
because inulin is filtered freely and the kidneys do not reabsorb or secrete
it. Inulin is a plant polysaccharide with a renal clearance value that is equal
to the GFR. When infused so the inulin plasma concentration is 1 mg/mL, this
means its plasma concentration (P) is 1 mg/mL. Usually, its urine
con-centration (U) is 125 mg/mL and its flow rate (V) is 1 mL/min. Its renal
clearance is calculated as:
C = (125 x 1) / 1 = 125 mL/min
This means that within one minute, the kidneys have cleared
all the inulin that was present in 125 mL of plasma. We can then determine how
the kidneys are handling the net amount of a certain substance.
There are three different outcomes to this deter-mination:
1. If the substance has a clearance value that is less than
the clearance value of inulin, the substance is reabsorbed.
2. If the renal clearance rate (C) is equal to that of
inulin, there is no net reabsorption or secretion of the substance.
3. If C is greater than that of insulin, the sub-stance is
secreted by the tubule cells into the filtrate. This usually occurs with most
drug metabolites.
It is essential to know a drug’s renal clearance rate. If
the rate is high, the drug dosage must also be high, and the drug must be
administered frequently to maintain therapeutic levels.