Humoral Immune Response
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Lymphatic System and Immunity
The humoral immune response involves B lympho-cytes. This response is provoked when a B cell encoun-ters its antigen. In the humoral immune response, antibodies specific for that antigen are manufactured.
Humoral
Immune Response
The humoral immune response involves B lympho-cytes. This
response is provoked when a B cell encoun-ters its antigen. In the humoral
immune response, antibodies specific for that antigen are manufactured.
Activation of B Cells
B cells may activate when encountering an antigen whose
shape fits the B cell’s antigen receptor shape, dividing repeatedly and
expanding its clone. However, B cells
usually require T cells to activate. T cells that encounter B cells bound to
identical foreign antigens release cytokines that
stimulate the B cells. The cyto-kines attract macrophages. Some of the B cell’s
clones differentiate into more memory
cells. These memory B cells respond quickly to reexposure to
specific anti-gens. Other B-cell clones differentiate into antibody- secreting
plasma cells, which can combine with their corresponding foreign antigens and
react against them (FIGURE
20-9). B cells can produce between 10 million and 1 billion
varieties of antibodies, each specific to an antigen. When the B cells are
prepared to undergo activation, they are described as being sensitized.
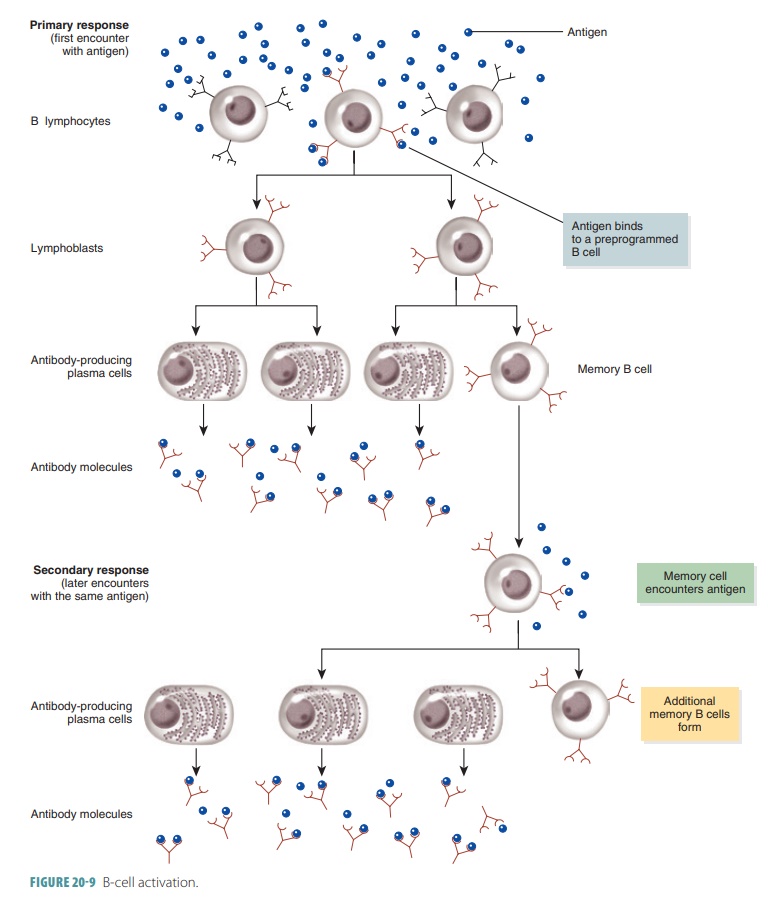
An antigen encountered by a B cell provokes the humoral immune response. As a result, antibodies thatare specific for that antigen develop. A naive, immu-nocompetent B lymphocyte becomes activated when its surface receptors are bound to matching antigens. Cross-linking occurs of the adjacent receptors. Most cloned cells differentiate into plasma cells, which are humoral response effector cells that secrete antibod-ies. They secrete antibodies at a rate of approximately 2,000 molecules every second. This activity continues for between four and five days before each plasma cell dies. The secreted antibodies have the identical antigen-binding properties as the receptor molecules of the parent B lymphocyte’s surface. These secreted antibodies circulate in blood or lymph. Memory cells develop from any clone cells that do not become plasma cells. If these cells encounter the same antigen later, they can cause a humoral response almost immediately.
Immunological Memory
A primary
immune response is constituted by acti-vation of B cells or T cells after
they first encounter the antigens for which they are specialized to react. This
usually occurs within three to six days. Over nearly this same period of time,
B cells specific for that antigen proliferate into approximately 12
generations. Plasma antibody levels increase after a mobilization period to
reach their peak within about 10 days and then decline (FIGURE 20-10). Plasma cells release antibodies
into the lymph. The antibodies are transported to the blood and throughout the
body to help destroy antigen-bearing agents. This continues for several weeks.
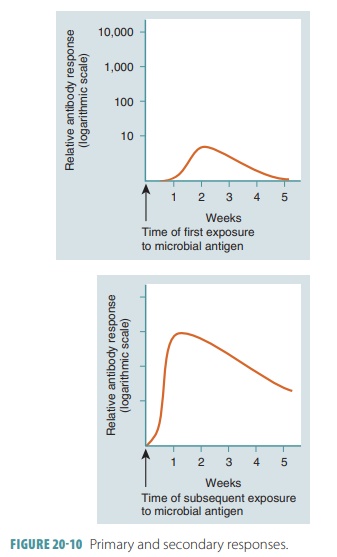
Some of the B cells then remain as memory cells so if the identical antigen is reencountered, clones of these memory cells enlarge and send antibodies to the antigen. These memory B cells, along with memory T cells, pro-duce a secondary immune response. After a primary immune response, detectable concentrations of antibod-ies appear in the blood plasma, usually five to 10 days after exposure to antigens, and a secondary immune response can then occur within one to two days. Memory cells live much longer than newly formed antibodies, which live between a few months and a few years. Secondary immune responses occur faster, with more effectiveness, than primary immune responses. They also last longer. The memory cells are “ready for action” because they were previously alerted to antigens. Therefore, these cells provide immunological memory.
Memory T
cells are produced in the same way ascytotoxic T cells. They do
not differentiate any more after an antigen triggers an immune response. When
the antigen appears again, however, memory T cells immediately differentiate
into cytotoxic T cells, which a fast and deadly response. Memory helper T cells are produced along with active helper T
cells.
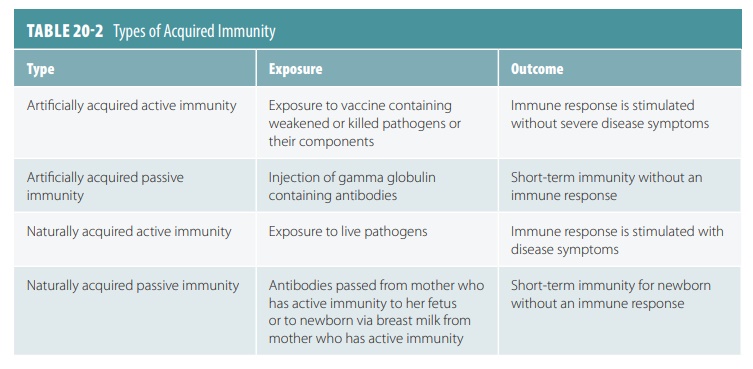
Active
Humoral Immunity
Active
humoral immunity is signified by antibodiesproduced by B cells
after encountering antigens. Active humoral immunity is acquired either naturally or arti-ficially. Examples of natural means of acquiring activehumoral
immunity include development of bacterial or viral infections, whereas examples
of artificial means of acquiring active humoral immunity include vaccines. Most vaccines contain
dead or attenuated pathogens or
components of them. The term “attenuated” means the pathogens are extremely
weakened but still alive. There are two major benefits of vaccines: they do not
cause most of the uncomfortable signs and symptoms that normally occur during
the primary response; and their weakened antigens provide immunogenic,
reac-tive functional determinants of antigens. During the primary response, the
level of antibody activity in the plasma, or antibody titer, does not peak until one to two weeks after the
initial exposure. TABLE
20-2 explains the various types of acquired
immunity.
Booster shots are vaccines that can intensify theimmune response when the same antigen is encoun-tered at a later time. Diseases that have been eradicated, nearly eradicated, or extremely weakened by vac-cines include smallpox, measles, polio, and whooping cough. In the United States, unfortunately, immu-nization of adults seems to be of less importance to many people than immunization of children. Even so, vaccines have greatly reduced serious outcomes from hepatitis B, influenza, pneumonia, and tetanus.
Passive
Humoral Immunity
Passive
humoral immunity involves the introduc-tion of antibodies into
the body. The B cells are not challenged by antigens, and immunological memory
does not occur. Therefore, the protection provided by the introduced antibodies
ends when they become nat-urally degraded. When antibodies from a mother cross
the placenta or are ingested through her milk, the fetus or infant is receiving
natural passive immunity. After
birth, the infant is protected for several months from all antigens that the
mother has been exposed to.
Artificial
passive immunity involves administration of exogenous antibodies such as gamma globulin, such as from the plasma of an immune
donor. These “outside” antibodies can be used to prevent hepatitis A, or to
treat conditions such as botulism, poisonous snake bites (in the form of an
antivenom), rabies, and tetanus (in the form of an antitoxin). Rapidly fatal
diseases such as these could be fatal before active immunity is able to be
established. Donated antibodies provide immedi-ate protection. However, they
only have a short-term effect, of between two and three weeks.
1. Explain how active humoral immunity may be acquired.
2. Describe how vaccines protect children against various
common illnesses.
3. Describe
how active and passive immunity differ.
1. What are the characteristics of adaptive immunity?
2. Explain the differences between a complete antigen and a hapten.
3. What is antigenic determination?
Related Topics