Mechanism of Drug Interactions
| Home | | Pharmacology |Chapter: Essential pharmacology : Drug Interactions
Drug interactions can be broadly divided into pharmacokinetic and pharmacodynamic interactions. In certain cases, however, the mechanisms are complex and may not be well understood.
MECHANISM OF DRUG INTERACTIONS
Drug interactions can
be broadly divided into pharmacokinetic and pharmacodynamic interactions. In certain cases, however, the mechanisms
are complex and may not be well understood. Few interactions take place even
outside the body when drug solutions are mixed before administration.
Pharmacokinetic Interactions
These interactions
alter the concentration of the object drug at its site of action (and
consequently the intensity of response) by affecting its absorption,
distribution, metabolism or excretion.
Pharmacokinetic Interaction
·
Alteration of absorption or first-pass metabolism
·
Displacement of plasma protein bound drug
· Alteration of drug binding to tissues affecting
volume of distribution and clearance
·
Inhibition/induction of metabolism
·
Alteration of excretion
Absorption Absorption of an orally administered drug can
be affected by other concurrently ingested drugs. This is mostly due to
formation of insoluble and poorly absorbed complexes in the gut lumen, as
occurs between tetracyclines and calcium/iron salts, antacids or sucralfate.
Phenytoin absorption is decreased by sucralfate due to binding in the g.i.
lumen. Such interactions can be minimized by adminstering the two drugs with a
gap of 2–3 hours so that they do not come in contact with each other in the
g.i.t. Ketoconazole absorption is reduced by H2 blockers and proton
pump inhibitors because they reduce gastric acidity which promotes dissolution
and absorption of ketoconazole. Antibiotics like ampicillin, tetracyclines,
cotrimoxazole markedly reduce gut flora that normally deconjugates oral contraceptive
steroids secreted in the bile as glucuronides and permits their enterohepatic
circulation. Several instances of contraceptive failure have been reported with
concurrent use of these
antibiotics due to lowering of the contraceptive blood levels.
Alteration of gut motility by atropinic drugs, tricyclic antidepressants, opioids
and prokinetic drugs like metoclopramide or cisapride can also affect drug
absorption.
Distribution Interactions involving drug distribution are
primarily due to displacement of one drug from its binding sites on plasma
proteins by another drug. Drugs highly bound to plasma proteins that have a
relatively small volume of distribution like oral anticoagulants, sulfonylureas,
certain NSAIDs and antiepileptics are particularly liable to displacement
interactions. Another requirement is that the displacing drug should bind to
the same sites on the plasma proteins with higher affinity. Displacement of bound
drug will initially raise the concentration of the free and active form of the
drug in plasma that may result in toxicity. However, such effects are usually
brief, because the free form rapidly gets distributed, metabolized and
excreted, so that steady-state levels are only marginally elevated. The
clinical outcome of displacement interactions is generally significant only
when displacement extends to tissue binding sites as well, or is accompanied by
inhibition of metabolism and/ or excretion. Quinidine has been shown to reduce
the binding of digoxin to tissue proteins as well as its renal and biliary
clearance by inhibing the efflux transporter P-glycoprotein, resulting in
nearly doubling of digoxin blood levels and toxicity.
Metabolism Certain drugs reduce
or enhance the rate of metabolism
of other drugs. They may thus affect the bioavailability (if the drug undergoes
extensive first pass metabolism in liver) and the plasma halflife of the drug (if
the drug is primarily eliminated by metabolism). Inhibition of drug metabolism
may be due to competition for the same CYP450 isoenzyme or cofactor, and
attains clinical significance mostly for drugs that are metabolized by
saturation kinetics. Macrolide antibiotics, azole antifungals, chloramphenicol,
omeprazole, SSRIs, HIV-protease inhibitors, cimetidine, ciprofloxacin and metronidazole
are some important inhibitors of metabolism of multiple drugs. Risk of statin
induced myopathy is increased by fibrates, niacin, erythromycin, azole
antifungals and HIV-protease inhibitors, probably due to inhibition of statin
metabolism. Because lidocaine metabolism is dependent on hepatic blood flow,
propranolol has been found to prolong its t½ by reducing blood flow to the
liver.
A number of drugs
induce microsomal drug metabolizing enzymes and enhance biotransformation of
several drugs (including their own in many cases). Induction involves gene
mediated increased synthesis of certain CYP450 isoenzymes; takes 1–2 weeks of
medication with the inducer to produce maximal effect (contrast inhibition of
metabolism which develops quickly) and regresses gradually over 1–3 weeks after
discontinuation of the inducer. Barbiturates, phenytoin, carbamazepine,
rifampin, cigarette smoking, chronic alcoholism and certain pollutants are
important microsomal enzyme inducers. Instances of failure of antimicrobial
therapy with metronidazole, doxycycline or chloramphenicol have occurred in
patients who are on long-term medication with an inducing drug. Contraceptive
failure and loss of therapeutic effect of many other drugs have occurred due to
enzyme induction. On the other hand, the toxic dose of paracetamol is lower in
chronic alcoholics and in those on enzyme inducing medication, because one of
the metabolites of paracetamol is responsible for its overdose hepatotoxicity.
Excretion Interaction involving excretion are important mostly in case of drugs actively
secreted by tubular transport mechanisms, e.g. probenecid inhibits tubular secretion
of penicillins and cephalosporins and prolongs their plasma t½. This is
particularly utilized in the single dose treatment of gonorrhoea. Aspirin
blocks the uricosuric action of probenecid and decreases tubular secretion of
methotrexate. Change in the pH of urine can also affect excretion of weakly
acidic or weakly basic drugs. This has been utilized in the treatment of
poisonings. Diuretics and to some extent tetracyclines, ACE inhibitors and certain
NSAIDs have been found to raise steadystate blood levels of lithium by promoting
its tubular reabsorption.
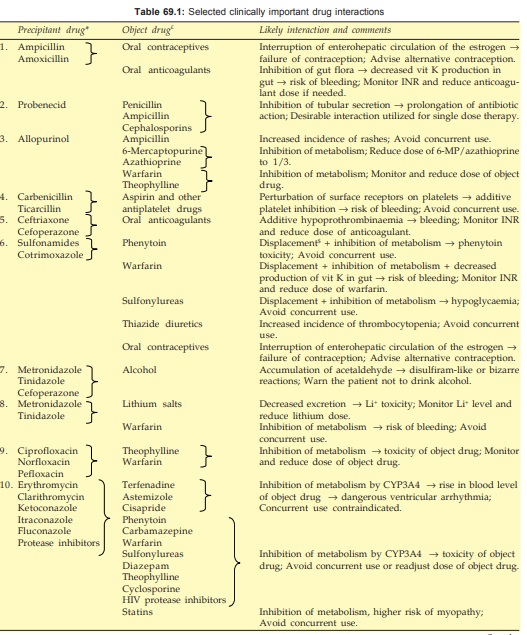
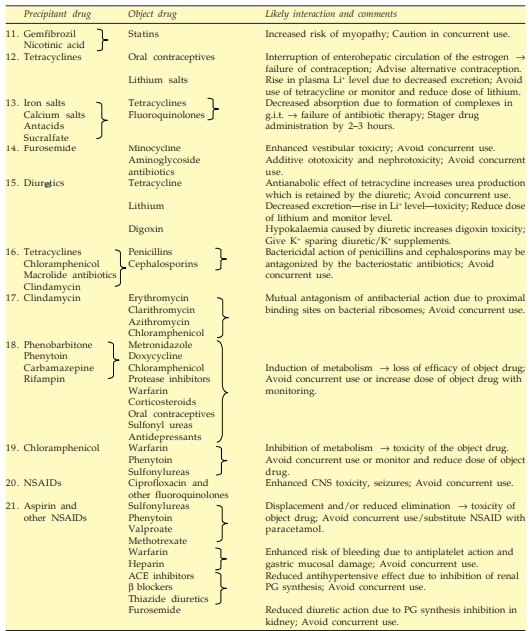
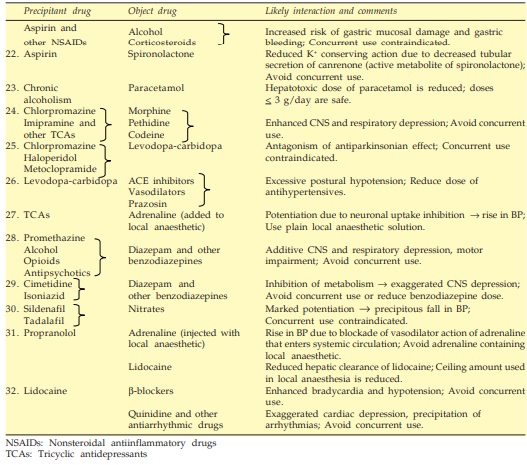
Pharmacodynamic Interactions
These interactions derive from modification of the action of one
drug at the target site by another drug, independent of a change in its concentration.
This may result in an enhanced response (synergism), an attenuated response
(antagonism) or an abnormal response. The phenomena of synergism and antagonism
are described in Chapter 4, and are deliberately utilized in therapeutics for
various purposes. Of clinical significance are the inadvertent concurrent
administration of synergistic or antagonistic pair of drugs with adverse
consequences. Some examples are:
· Excessive sedation, respiratory depression, motor incoordination due to concurrent administration of a benzodiazepine (diazepam), a sedating antihistaminic (promethazine), a neuroleptic (chlorpromazine), an opioid (morphine) or drinking alcoholic beverage while taking any of the above drugs.
· Excessive fall in BP and fainting due to
concurrent administration of α1 adrenergic blockers,
vasodilators, ACE inhibitors, high ceiling diuretics and cardiac depressants.
· Pronounced and asymptomatic hypoglycaemia can
occur when propranolol is administered to diabetics receiving insulin/
sulfonylureas, due to blockade of β adrenoceptors which contribute to recovery
from hypoglycaemia as well as some hypoglycaemic symptoms.
· Additive prolongation of prothrombin time and
bleeding by administration of ceftriaxone or cefoperazone to a patient on oral
anticoagulants.
· Excessive platelet inhibition resulting in
bleeding due to simultaneous use of aspirin/ticlopidine/clopidogrel and carbenicillin.
· Increased risk of bleeding due to concurrent
use of antiplatelet drugs (aspirin, clopidogrel) with anticoagulants
(warfarin).
· Marked bradycardia due to administration of
propranolol in digitalized patients.
· Precipitous fall in BP and myocardial
ischaemia due to use of sildenafil by patients receiving organic nitrates,
because nitrates increase generation of c-GMP,while sildenafil prevents its
degradation by inhibiting PDE 5.
· Severe hyperkalaemia by concurrent use of ACE
inhibitors and K+ sparing diuretics.
· Additive ototoxicity due to use of an aminoglycoside
antibiotic in a patient receiving furosemide.
· Antagonism of bactericidal action of βlactam antibiotic by
combining it with a bacteriostatic drug like tetracycline, erythromycin or clindamycin.
· Mutual antagonism of antibacterial action of
macrolides, clindamycin and chloram phenicol due to interference with each
other’s binding to the bacterial 50S ribosome.
· Reduction in antihypertensive action of
clonidine by chlorpromazine and imipramine, possibly due to blockade of central
action of clonidine.
· Attenuation of antihypertensive effect of ACE
inhibitors/β blockers/diuretics by
NSAIDs due to inhibition of renal PG synthesis.
· Blunting of K+ conserving action of spironolactone
by aspirin, because it inhibits the tubular secretion of canrenone (an active
metabolite of spironolactone).
· Blockade of antiparkinsonian action of
levodopa by neuroleptics and metoclopramide having antidopaminergic action.
Abnormal responses
sometimes result from pharmacodynamic interaction between certain drugs, e.g.
metronidazole and cefoperazone inhibit the enzyme aldehyde dehydrogenase
resulting in bizarre distressing symptoms if the patient drinks alcohol. The
basis of certain interactions is not explained, e.g. ampicillin has produced
high incidence of skin rashes in patients treated with allopurinol.
Drug Interactions Before Administration
Certain drugs react with
each other and get inactivated if their solutions are mixed before administration.
In combined oral or parenteral formulations, the manufacturers take care that
such incompatibilities do not take place. In practice situations, these in vitro interactions occur when
injectable drugs are mixed in the same syringe or infusion bottle. Some
examples are:
· Penicillin G or
ampicillin mixed with gentamicin or another aminoglycoside antibiotic.
· Thiopentone sodium
when mixed with succinylcholine or morphine.
· Heparin when mixed
with penicillin/ gentamicin/hydrocortisone.
· Noradrenaline when
added to sodium bicarbonate solution.
