Peripherally Acting Muscle Relaxants
| Home | | Pharmacology |Chapter: Essential pharmacology : Skeletal Muscle Relaxants
Skeletal muscle relaxants are drugs that act peripherally at neuromuscular junction/ muscle fibre itself or centrally in the cerebrospinal axis to reduce muscle tone and/or cause paralysis.
PERIPHERALLY ACTING MUSCLE
RELAXANTS
I. Neuromuscular
blocking agents
A. Nondepolarizing (Competitive)
blockers
a)
Long acting:
dTubocurarine,
Pancuronium, Doxacurium, Pipecuronium
b) Intermediate acting:
Vecuronium, Atracurium, Cisatracurium, Rocuronium, Rapacuronium
c)
Short acting:
Mivacurium
B. Depolarizing blockers
Succinylcholine (SCh.,
Suxamethonium), Decamethonium (C10)
II. Directly acting agents
Dantrolene sodium
Quinine
Note:
1. Metocurine and Alcuronium are analogues of dtubocurarine no longer in clinical
use. Gallamine is also obsolete.
2. Aminoglycoside,
tetracycline, polypeptide antibiotics interfere with neuromuscular transmission
at high doses, but are not employed as muscle relaxants.
Neuromuscular Blocking Agents
Curare
It is the generic name
for certain plant extracts used by south American
tribals as arrow poison for game hunting. The animals got paralysed even if not
killed by the arrow. Natural sources of curare are Strychnos toxifera, Chondrodendron
tomentosum and related plants. Muscle
paralysing active principles of these are tubocurarine, toxiferins, etc.
Tubocurarine was first
clinically used in 1930s; many synthetic compounds including Succinylcholine were introduced subsequently.
Search has continued for neuromuscular blockers to provide greater
cardiovascular stability during surgery and for drugs with differing onset and
duration of action to suit specific requirements. The latest additions are doxacurium, pipecuronium, rocuronium, mivacurium, rapacuronium and cisatracurium.
Mechanism Of Action
The site of action of
both competitive and depolarizing blockers is the end plate of skeletal muscle
fibres.
Competitive Block (Nondepolarizing Block)
This is produced by curare and related drugs. Claude Bernard
(1856) precisely localized the site of action of curare to be the neuromuscular
junction. He stimulated the sciatic nerve of pithed frog and recorded the
contractions of gastrocnemius muscle. Injection of curare in the ventral lymph
sac caused inhibition of muscle twitches but there was no effect if the blood
supply of the hind limb was occluded. This showed that curare acted
peripherally and not centrally. Soaking a portion of the sciatic nerve in
curare solution did not affect the twitches and a curarized muscle still
responded to direct stimulation—thus, nervous conduction and muscle contraction
were intact. The only possible site of action could be the neuromuscular
junction. This has now been confirmed by close iontophoretic application of dTC
to the muscle end plate and by other modern techniques.
The competitive
blockers have affinity for the nicotinic (NM) cholinergic receptors
at the muscle end plate, but have no intrinsic activity. The NM
receptor has been isolated and studied in detail. It is a protein with 5
subunits (α2 β ε or γ and δ) which are arranged
like a rosette surrounding the Na+ channel. The two α subunits carry two ACh
binding sites; these have negatively charged groups which combine with the
cationic head of ACh → opening of Na+ channel. Most of
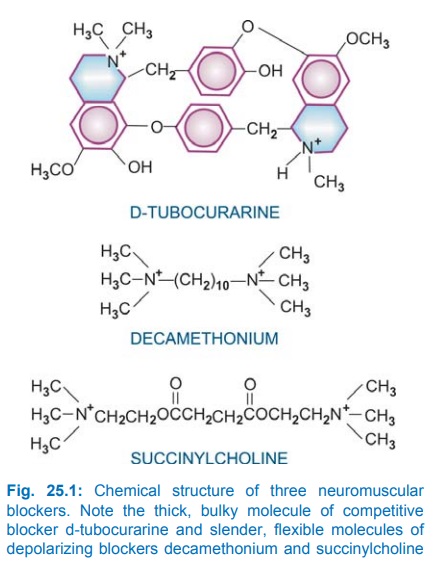
the competitive blockers have two or more quaternary N+ atoms (Fig.
25.1) which provide the necessary attraction to the same site, but the bulk of
the antagonist molecule does not allow conformational changes in the subunits
needed for opening the channel. Competitive blockers generally have thick bulky
molecules and were termed Pachycurare
by Bovet (1951). ACh released from motor nerve endings is not able to combine
with its receptors to generate end plate potential (EPP). dTC thus reduces the
frequency of channel opening but not its duration or the conductance of a
channel once it has opened. When the magnitude of EPP falls below a critical
level, it is unable to trigger propagated muscle action potential (MAP) and muscle
fails to contract in response to nerve impulse. The antagonism is surmountable
by increasing the concentration of ACh in
vitro and by anticholinesterases in
vivo. At very high concentrations, curare like drugs enter the Na+
channels and directly block them to produce more intense noncompetitive neuromuscular
block that is only partly reversed by neostigmine.
The competitive
blockers also block prejunctional nicotinic receptors located on motor nerve
endings. Since activation of these receptors by ACh normally facilitates
mobilization of additional quanta of ACh from the axon to the motor nerve
endings, their blockade contributes to depression of neuromuscular
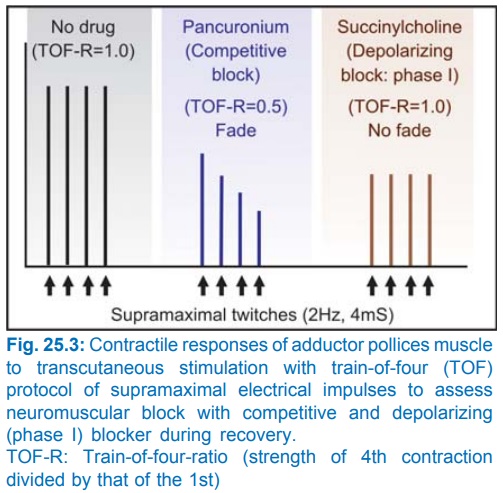
transmission. Accordingly, the competitive blockers exhibit the ‘fade’ phenomenon
(Fig. 25.3), i.e. twitch responses during partial block are progressively
depressed on repetitive stimulation.
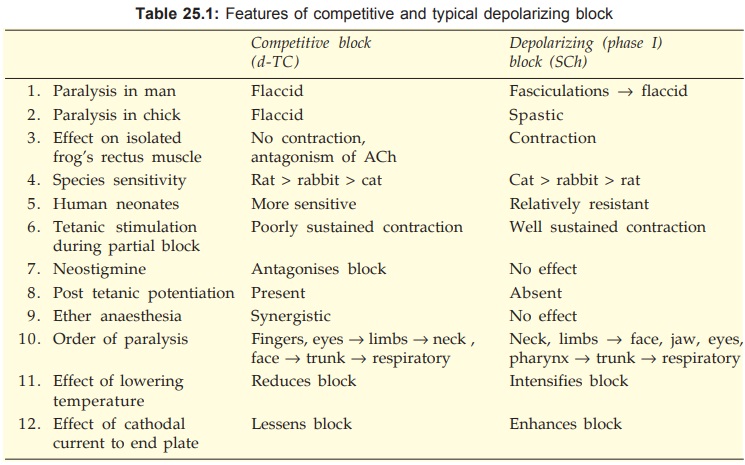
Depolarizing Block
Decamethonium and SCh have affinity as well as submaximal intrinsic
activity at the NM cholinoceptors. They depolarize muscle end plates
by opening Na+ channels (just as ACh does) and initially produce
twitching and fasciculations. Because in the focally innervated mammalian
muscle, stimulation is transient; longer lasting depolarization of muscle end
plate produces repetitive excitation of the fibre. In the multiplely innervated
contracture muscle (rectus abdominis of frog) stimulation is prolonged
resulting in sustained contraction. These drugs do not dissociate rapidly from
the receptor → induce prolonged
partial depolarization of the region around muscle end plate → Na+
channels get inactivated (because transmembrane potential drops to about –50
mV) → ACh released from
motor nerve endings is unable to generate propagated MAP → flaccid paralysis in
mammals. In other words a zone of inexcitability is created round the end plate
preventing activation of the muscle fibre. In birds, the area of depolarization
is more extensive and spastic paralysis occurs.
Depolarizing blockers
also have 2 quaternary N+ atoms, but the molecule is long, slender
and flexible—termed Leptocurare by
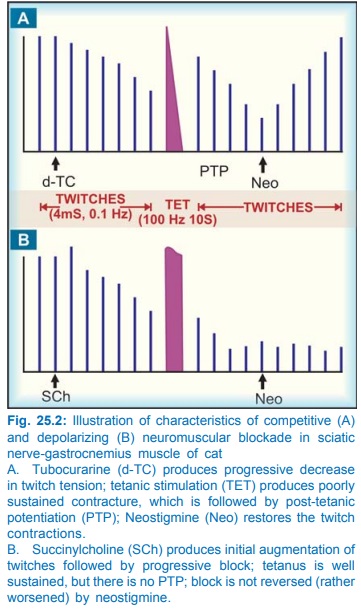
Bovet. The features of classical depolarizing block differ markedly from that
of nondepolarizing block (see Fig.
25.2 and Table 25.1).
However, in many
species, e.g. dog, rabbit, rat, monkey, in slow contracting soleus muscle of
cat, and under certain conditions in man the depolarizing agents produce dual
mechanism neuromuscular blockade which can be divided into two phases:
Phase I Block
It is rapid in onset,
results from persistent
depolarization of muscle end plate and has features of classical depolarization
blockade. This depolarization declines shortly afterwards and repolarization
occurs gradually despite continued presence of the drug at the receptor, but
neuromuscular transmission is not restored and phase II block supervenes.
Phase II Block
It is slow in onset
and results from desensitization
of the receptor to ACh. No. It, therefore, superficially resembles block produced
by dTC: membrane is nearly repolarized, recovery is slow, contraction is not
sustained during tetanic stimulation and the block is partially reversed by
anticholinesterases.
In man and fast
contracting muscle (tibialis anterior) of cat, normally only phase I block is
seen. Phase II block may be seen in man when fluorinated anaesthetics have been
given or when SCh is injected in high dose or infused continuously. SCh readily
produces phase II block in patients with atypical or deficient pseudocholinesterase.
Actions
Skeletal Muscles
Intravenous injection
of nondepolarizing
blockers rapidly produces muscle weakness followed by flaccid paralysis. Small
fast response muscles (fingers, extraocular) are affected first; paralysis
spreads to hands, feet—arm, leg, neck, face—trunk—intercostal muscles—finally
diaphragm: respiration stops. The rate of attainment of peak effect and the
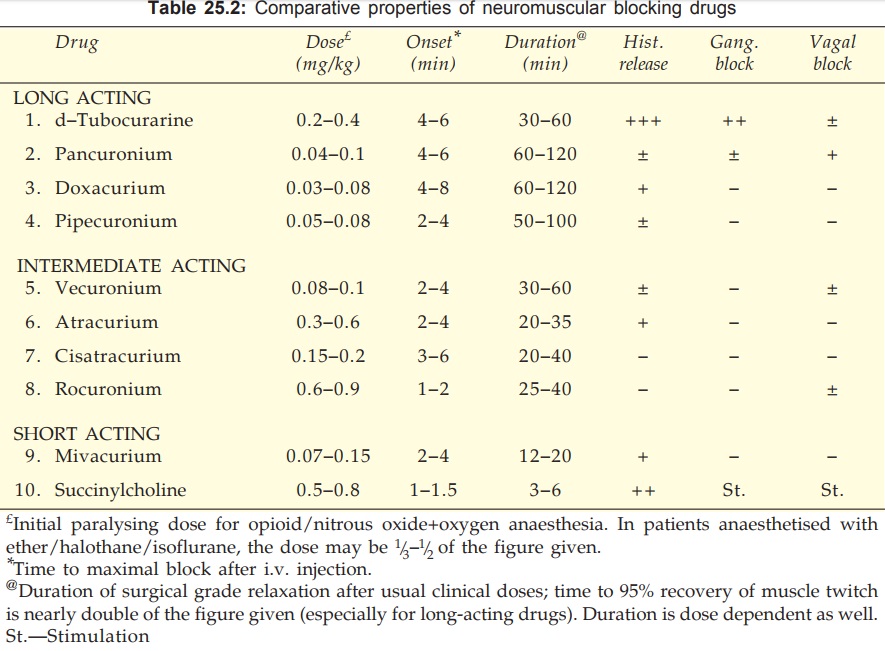
duration for which it is maintained depends on the drug (Table 25.2), its dose,
anaesthetic used, haemodynamic, renal and hepatic status of the patient and
several other factors. Recovery occurs in the reverse sequence; diaphragmatic
contractions resume first.
Depolarizing blockers
typically produce fasciculations lasting a few seconds before inducing flaccid
paralysis, but fasciculations are not prominent in well-anaesthetized patients.
Though the sequence in which muscles are involved is somewhat different from
the competitive blockers (Table 25.1), the action of SCh develops with such rapidity
that this is not appreciated. Apnoea generally occurs within 45–90 sec, but
lasts only 2–5 min; recovery is rapid.
Clinical Monitoring Of Neuromuscular Block
In anaesthetic
practice neuromuscular block (especially during recovery) is monitored by recording
contractile responses of thumb muscles to transcutaneous ulnar nerve
stimulation. Since single twitch responses have to be interpreted in comparison
to twitches before the blocker and are not reliable, the preferred method is
‘trainoffour’ (TOF) protocol. Four supramaximal electrical stimuli are applied
at 2Hz and contractions of thumb muscle are recorded (Fig. 25.3). The TOFratio
is obtained by dividing the strength of 4th contraction by that of the 1st. In
the untreated subject all the 4 contractions remain equal and TOFratio is 1.0.
During partial
competitive block (as during onset and recovery or reversal) the degree of
block corresponds to the decrease in TOFratio, because competitive blockers
exhibit ‘fade’ phenomenon. As the muscles recover, the TOFratio improves and
becomes 1.0 at complete recovery.
On the other hand,
classical or phaseI depolarizing block does not exhibit fade; the TOFratio
remains 1.0, though all the 4 twitches are depressed equally depending on the
degree of block. Fade is again seen when phase II or desensitization block
occurs with prolonged use of a depolarizing agent and TOFratio is depressed as
in the case of competitive block. However, SCh generally requires no
monitoring.
Other protocols used
in clinical monitoring of neuromuscular block are ‘double burst’, ‘tetanic
stimulation’ and ‘posttetanic count’ methods.
Autonomic Ganglia
Because the cholinergic
receptors in autonomic ganglia are nicotinic (though of a different subclass NN),
competitive neuromuscular blockers produce some degree of ganglionic blockade;
dTC has the maximum propensity in this regard, while the newer drugs are
practically devoid of it. SCh may cause ganglionic stimulation by its agonistic
action on nicotinic receptors.
Histamine Release
dTC releases histamine from mast cells. This does not involve immune
system and is due to the bulky cationic nature of the molecule. Histamine
release contributes to hypotension produced by dTC; flushing, bronchospasm and increased
respiratory secretions are other effects. Intradermal injection of dTC produces
a wheal similar to that produced by injecting histamine. Histamine releasing
potential of other neuromuscular blockers is graded in Table 25.2.
Heparin may also be simultaneously
released from mast cells.
C.V.S.
dTubocurarine produces
significant fall in BP. This is due to—
a)
ganglionic blockade
b) histamine release and
c)
reduced venous return—a result of paralysis of
limb and respiratory muscles.
Heart rate may increase due to vagal ganglionic blockade.
Pancuronium and vecuronium also tend to cause tachycardia. All newer nondepolarizing
drugs have negligible effects on BP and HR.
Cardiovascular effects of SCh are variable. Generally
bradycardia occurs initially due to activation of vagal ganglia followed by
tachycardia and rise in BP due to stimulation of sympathetic ganglia. BP
occasionally falls on account of its muscarinic action causing vasodilatation.
Prolonged administration of SCh has caused cardiac arrhythmias and even arrest
in patients with burns, soft tissue injury and tetanus. Efflux of intracellular
K+ occurs in these conditions which is augmented by prolonged
depolarization of skeletal muscles.
G.I.T.
The ganglion blocking
activity of competitive blockers
may enhance postoperative paralytic ileus after abdominal operations.
C.N.S.
All neuromuscular
blockers are quaternary compounds—do not cross blood-brain barrier. Thus, on
i.v. administration no central effects follow. However, dTC applied to brain
cortex or injected in the cerebral ventricles produces strychnine like effects.
Pharmacokinetics
All neuromuscular
blockers are polar quaternary compounds—not absorbed orally, do not cross cell
membranes, have low volumes of distribution and do not penetrate placental or
blood-brain barrier. They are practically always given i.v., though i.m.
administration is possible. Muscles with higher blood flow receive more drug
and are affected earlier. Redistribution to nonmuscular tissues plays a
significant role in the termination of surgical grade muscle relaxation, but
residual block may persist for a longer time depending on the elimination t½.
The duration of action of competitive blockers is directly dependent on the
elimination t½. Drugs that are primarily metabolized in the plasma/liver, e.g.
vecuronium, atracurium, rocuronium, and mivacurium have relatively shorter t½
and duration of action (20–40 min), while those largely excreted by the kidney,
e.g. pancuronium, dTc, doxacurium and pipecuronium have longer t½ and duration
of action (>60 min). With repeated administration redistribution sites are
filled up and duration of action is prolonged. The unchanged drug is excreted
in urine as well as in bile.
SCh is rapidly hydrolysed
by plasma pseudocholinesterase to succinylmonocholine and then succinic acid +
choline (action lasts 3–5 min). Some patients have genetically determined
abnormality (low affinity for SCh) or deficiency of pseudocholinesterase. In
them, SCh causes dominant phase II blockade resulting in muscle paralysis and
apnoea lasting hours, because SCh is a poor substrate for the more specific
AChE found at the motor end plate.
Notes On Individual Compounds
d-Tubocurarine
Because of its
prominent histamine releasing, ganglion
blocking and cardiovascular actions as well as long duration of paralysis
needing pharmacological reversal, dTC is not used now.
Succinylcholine
Despite its propensity
to cause muscle
fasciculations and soreness, changes in BP and HR, arrhythmias, histamine
release and K+ efflux from muscles → hyperkalaemia and its
complications, SCh is the most commonly used muscle relaxant for passing
tracheal tube. It induces rapid, complete and predictable paralysis with
spontaneous recovery in ~5 min. Excellent intubating condition viz. relaxed jaw, vocal cords apart and
immobile with no diaphragmatic movements, is obtained within 1–1.5 min.
Occasionally it is used by continuous i.v. infusion for producing controlled
muscle relaxation of longer duration. It should be avoided in younger children
unless absolutely necessary, because risk of hyperkalaemia and cardiac
arrhythmia is higher. Risk of regurgitation and aspiration of gastric contents
is increased by SCh in GERD patients and in the obese, especially if stomach is
full. Infants require higher per kg dose.
MIDARINE, SCOLINE, MYORELEX, ENTUBATE 50 mg/ml inj, 2 ml amp.
Pancuronium
A synthetic steroidal compound, ~5 times more potent than dTC;
provides good cardiovascular stability (little ganglionic blockade), seldom
induces flushing, bronchospasm or cardiac arrhythmias because of lower
histamine releasing potential. Rapid i.v. injection may cause rise in BP and
tachycardia due to vagal blockade and NA release. It is primarily eliminated by
renal excretion. Because of longer duration of action, frequently needing
reversal, its use is now restricted to prolonged operations, especially
neurosurgery.
PAVULON, PANURON, NEOCURON 2 mg/ml in 2 ml amp.
Doxacurium
A bis-quaternary muscle relaxant having the least rapid
onset and the longest action: suitable for long duration surgeries. It is
primarily eliminated by kidney, though hepatic metabolism also occurs.
Cardiovascular changes are minimal.
Pipecuronium
Another muscle
relaxant with a slow onset and
long duration of action; steroidal in nature; recommended for prolonged
surgeries. It exerts little cardiovascular action, though transient hypotension
and bradycardia can occur. Elimination occurs through both kidney and liver.
ARDUAN 4 mg/2 ml inj.
Vecuonium
A close congener of pancuronium
with a shorter duration of action due to rapid distribution and metabolism.
Recovery is generally spontaneous not needing neostigmine reversal unless
repeated doses have been given. Cardiovascular stability is still better due to
lack of histamine releasing and ganglionic action; tachycardia sometimes
occurs. Currently, it is the most commonly used muscle relaxant for routine
surgery.
NORCURON 4 mg amp,
dissolve in 1 ml solvent supplied.
NEOVEC 4 mg amp, 10 mg
vial.
Atracurium
A bis-quaternary competitive blocker, 4 times less potent than pancuronium
and shorter acting: reversal is mostly not required. The unique feature of
atracurium is inactivation in plasma by spontaneous nonenzymatic degradation
(Hofmann elimination) in addition to that by cholinesterases. Consequently its
duration of action is not altered in patients with hepatic/renal insufficiency
or hypodynamic circulation. It is the preferred muscle relaxant for such patients
as well as for neonates and the elderly. Hypotension may occur due to histamine
release.
TRACRIUM 10 mg/ml inj
in 2 ml vial.
Cisatracurium
This RCis, RCis enantiomer of atracurium is nearly 4
times more potent, slower in onset, but similar in duration of action. Like
atracurium it undergoes Hofmann elimination, but in contrast it is not hydrolysed
by plasma cholinesterase. Most importantly, it does not provoke histamine
release.
Side effects are
fewer.
Rocuronium
A new
non-depolarizing blocker with a rapid
onset and intermediate duration of action which can be used as alternative to
SCh for tracheal intubation without the disadvantages of depolarizing block and
cardiovascular changes. The same drug also serves as maintenance muscle
relaxant, seldom needing reversal. The onset of action is dose-dependent; intubating
conditions are attained in 90 sec with 0.6 mg/kg, but within 60 sec at 1.0
mg/kg. Within limits, the duration of paralysis is also dose-dependent. This
neuromuscular blocker is gaining popularity for its versatility and more
precisely timed onset and duration of action. Infused i.v. (0.3–0.6
mg/kg/hour), it is also being used to facilitate mechanical ventilation in
intensive care units. It is eliminated mainly by liver. Mild vagolytic action
increases HR somewhat.
CUROMID 50 mg/ml, 100 mg/10
ml vials.
Mivacurium
It is the shortest acting
competitive blocker; does not need
reversal. Dose and speed of injection related transient cutaneous flushing can
occur due to histamine release. Fall in BP is possible, but change in HR is
minimal. It is metabolized rapidly by plasma cholinesterases: prolonged
paralysis can occur in pseudocholinesterase deficiency.
Interactions
1. Thiopentone sod and SCh solutions should not be mixed in the same syringe—react
chemically.
2. General Anaesthetics potentiate competitive blockers; ether in particular as well as fluorinated hydrocarbons.
Isofluorane potentiates more than halothane. Nitrous oxide potentiates the
least. Ketamine also intensifies nondepolarizing block. Fluorinated
anaesthetics predispose to phase II blockade by SCh. Malignant hyperthermia produced
by halothane and isoflurane in rare individuals (genetically predisposed) is
more common in patients receiving SCh as well.
3. Anticholinesterases reverse the action of competitive blockers. Neostigmine
0.5–2 mg i.v. is almost routinely used after pancuronium and other long acting
blockers to hasten recovery at the end of operation. Though it also reverses
ganglionic blockade to some extent, hypotension and bronchospasm can occur due
to muscarinic action of neostigmine; this can be prevented by prior atropinization.
Pretreatment with H1 antihistamines reduces hypotension due to dTC
and others which release histamine.
4. Antibiotics Aminoglycoside antibiotics reduce ACh release from prejunctional nerve endings by competing
with Ca2+. They interfere with mobilization of ACh containing
vesicles from a central location to near the terminal membrane, and have a weak
stabilizing action on the postjunctional membrane. In clinically used doses,
they do not by themselves produce muscle relaxation, but potentiate competitive
blockers. The dose of competitive blocker should be reduced in patients
receiving high doses of these antibiotics. Application of streptomycin powder
locally at the end of bowel surgery has caused prolonged apnoea if a
competitive blocker had been used during the operation. Tetracyclines (by
chelating Ca2+), polypeptide antibiotics, clindamycin and lincomycin
also synergise with competitive blockers.
5.
Calcium Channel Blockers Verapamil and others potentiate both competitive and
depolarizing neuromuscular blockers.
6.
Diuretics produce hypokalemia
which enhances competitive block.
7. Diazepam, propranolol and quinidine intensify competitive
block, while high dose of corticosteroids reduces it.
Toxicity
a) Respiratory paralysis
and prolonged apnoea is the most important problem.
b) Flushing is common
with dTC, can occasionally occur with atracurium and mivacurium, rare with
others.
c) Fall in BP and
cardiovascular collapse can occur, especially in hypovolemic patients. This is
less likely with the newer drugs. Muscle relaxants should be used with great
caution in patients with severe hepatic and renal disease.
d) Cardiac arrhythmias
and even arrest have occurred, especially with SCh, particularly in digitalized
patients. SCh releases K+ from muscles: can cause dangerous
hyperkalaemia, especially in patients with extensive burns and soft tissue
injuries.
e) Precipitation of
asthma with dTC and other histamine releasing neuromuscular blockers.
f) Postoperative muscle
soreness may be complained after SCh.
Uses
1. The most important
use of neuromuscular blockers is as adjuvants to general anaesthesia; adequate
muscle relaxation can be achieved at lighter planes. Many surgical procedures
are performed more safely and rapidly by employing muscle relaxants. Muscle relaxants
also reduce reflex muscle contraction in the region undergoing surgery, and
assist maintenance of controlled ventilation during anaesthesia. They are
particularly helpful in abdominal and thoracic surgery, intubation and
endoscopies, orthopedic manipulations, etc.
SCh is employed for brief procedures, e.g. endotracheal
intubation, laryngoscopy, broncho scopy, esophagoscopy, reduction of fractures,
dislocations, and to treat laryngospasm. For ocular surgery competitive
blockers are preferred as they paralyse extraocular muscles at doses which have
little effect on larger muscles. Other factors which should be considered in
selecting the relaxant are—onset of action, duration of blockade required,
cardiovascular effects of the drug as well as patient’s hepatic, renal and
haemodynamic status.
2. Assisted ventilation: Critically ill patients in intensive
care units often need ventilatory support. This can be facilitated by
continuous infusion of a competitive neuromuscular blocker which reduces the
chest wall resistance to inflation.
3. Convulsions and trauma from electroconvulsive therapy can be
avoided by the use of muscle relaxants without decreasing the therapeutic
benefit. SCh is most commonly used for this purpose. The short acting competitive
blocker mivacurium is an alternative.
4. Severe cases of tetanus and status
epilepticus, which are not controlled by diazepam or other drugs, may be paralysed
by a neuromuscular blocker (repeated doses of a competitive blocker) and maintained
on intermittent positive pressure respiration till the disease subsides.
Directly Acting Muscle Relaxants
Dantrolene
This muscle relaxant
is chemically and pharmacologically
entirely different from neuromuscular blockers: effect superficially resembles
that of centrally acting muscle relaxants. Neuromuscular transmission or MAP
are not affected, but muscle contraction is uncoupled from depolarization of
the membrane. Dantrolene acts on the RyR (Ryanodine Receptor) calcium channels
in the sarcoplasmic reticulum of skeletal muscles and prevents their depolarization
triggered opening. Intracellular release of Ca2+ needed for
excitation-contraction coupling is interfered with. Fast contracting ‘twitch’
muscles are affected more than slow contracting ‘antigravity’ muscles.
Dantrolene is slowly
but adequately absorbed from the g.i.t. It penetrates brain and produces some
sedation, but has no selective effect on polysynaptic reflexes responsible for
spasticity. It is metabolized in liver and excreted by kidney with a t½ of 8–12
hours.
Used orally dantrolene
(25–100 mg QID) reduces spasticity in upper motor neurone disorders,
hemiplegia, paraplegia, cerebral palsy and multiple sclerosis. However, it also
reduces voluntary power; the resulting weakness considerably neutralizes the
benefit.
Used i.v. (1 mg/kg
repeated as required) it is the drug of choice for malignant hyperthermia which
is due to persistent release of Ca2+ from sarcoplasmic reticulum
(induced by fluorinated anaesthetics and SCh in genetically susceptible individuals
with abnormal RyR, see p. 372). Some
benefit may also be obtained in neuroleptic malignant syndrome, though this
reaction does not appear to be due to abnormal Ca2+ release in
muscles.
Adverse Effects
Muscular weakness is
the dose limiting side effect.
Sedation, malaise, light headedness and other central effects occur, but are
less pronounced than with centrally acting muscle relaxants. Troublesome
diarrhoea is another problem. Long term use causes dose dependent serious liver
toxicity in 0.1–0.5% patients. This has restricted its use in chronic
disorders.
Quinine
It increases
refractory period and decreases
excitability of motor end plates. Thus, responses to repetitive nerve
stimulation are reduced. It decreases muscle tone in myotonia congenita. Taken
at bed time (200– 300 mg) it may abolish nocturnal leg cramps in some patients.
Related Topics
