Bisphosphonates
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Calcium Balance
Bisphosphonates (BPNs) are analogues of pyrophosphate: carbon atom replacing oxygen in the POP skeleton. They inhibit bone resorption and have recently attracted considerable attention because of their ability to prevent osteoporosis in addition to their usefulness in metabolic bone diseases and hypercalcaemia.
BISPHOSPHONATES
Bisphosphonates (BPNs) are analogues of pyrophosphate: carbon
atom replacing oxygen in the POP skeleton. They inhibit bone resorption and
have recently attracted considerable attention because of their ability to
prevent osteoporosis in addition to their usefulness in metabolic bone diseases
and hypercalcaemia. They are the most effective antiresorptive drugs.
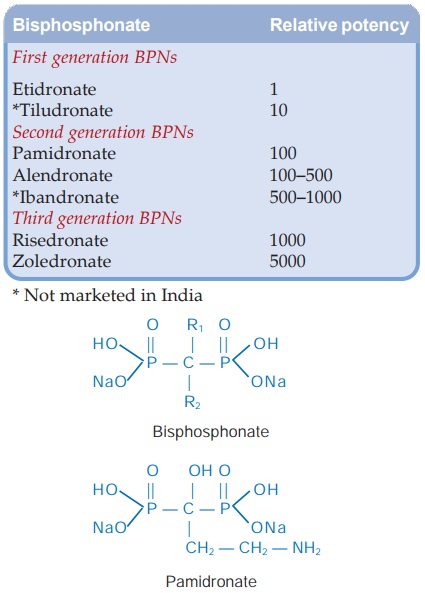
Chronologically and according to potency, the BPNs can be grouped into 3
generations (see box). The first
generation compounds have simpler side chains, are the least potent and seldom
used now. The second and third generation compounds have an amino or
nitrogenous ring substitution in the side chain, are more potent, have higher
efficacy and additional mode of action.
The mechanism of
action of BPNs is not fully understood, but two facets of action have been
delineated:
(a) BPNs have strong
affinity for calcium phosphate: have selective action in calcified tissue. The
two main components of bone are protein matrix and the solid mineral phase
(hydroxyapatite). On the surface of resorptive pits the mineral phase is
solubilized in the clear acidic zone created at the ruffled border of
osteoclasts, followed by resorption of protein matrix in this area by acid
hydrolases secreted from osteoclasts. BPNs localise in the acidic zone under
the osteoclasts due to their high affinity for Ca2+ ions. When Ca2+ ions are
released from the bone surface due to high acidity, the BPNs are also released
and are internalized into osteoclasts by endocytosis. This results in:
• Accelerated
apoptosis of osteoclasts reducing their number.
• Disruption of
cytoskeleton and ruffled border of osteoclasts.
In addition, BPNs appear
to affect osteoclast precursors and inhibit their differentiation by suppressing
IL6.
(b) It has been shown
recently that BPNs, especially the second and third generation potent amino-derivatives
like alendronate, zoledronate, have important metabolic effects in the mevalonate
pathway for isoprenoid lipid synthesis. They inhibit prenylation of certain GTP-binding
proteins involved in cytoskeletal organization, membrane ruffling and vesicle
movement. The net result is inactivation of osteoclasts, impaired vesicle
fusion and enhanced apoptosis. Interference with mevalonate pathway may also
impart antitumor action on bony metastasis.
All oral BPNs are
poorly absorbed, and produce gastric irritation, esophagitis as the major side
effect. They are contraindicated in gastroesophageal reflux, peptic ulcer and
renal impairment.
The BPNs are useful in
conditions characterized by enhanced bone turnover.
1. Osteoporosis The second and third generation BPNs (e.g. alendronate,
risedronate) are effective in preventing and treating postmenopausal osteoporosis
in women as well as age related, idiopathic and steroidinduced osteoporosis in
both men and women. Alendronate has been found equally or more effective than
HRT or raloxifene in conserving bone mineral density and has reduced the risk
of vertebral as well as hip fracture by 47–56%.
Estrogens prevent
vertebral but not other fractures. BPNs are more effective than calcitonin and
continue to afford protection for at least 5 years of continuous use.
2. Paget’s
Disease This disease due to
abnormal osteoclast function producing disordered bone remodeling and honeycomblike
bone architecture is benefited by BPNs. They arrest osteolytic lesions, reduce
bone pain and improve secondary symptoms. Longlasting remissions may be
induced. Alendronate, risedronate, pamidronate and zoledronate are used now. They
are more convenient, more effective and cheaper than calcitonin. Combined use
of BPNs and calcitonin further increases efficacy. Treatment with BPNs should
not exceed 6 months; but courses may be repeated after a gap.
3. Hypercalcaemia
Of Malignancy Severe hypercalcaemia, a common complication of
malignancy, is a medical emergency with altered consciousness. Pamidronate
(60–90 mg i.v. over 2–4 hours) or zoledronate (4 mg i.v. over 15 min) are the
most effective drugs, but take 24–48 hours to act. They may be supplemented by
i.m. calcitonin 6–12 hourly for 2 days for rapid action. Vigorous i.v.
hydration along with furosemide to prevent volume over load is started before
BPN infusion. It reduces serum calcium within few hours and corrects the
attending dehydration. Oral BPNs are not useful.
4. Osteolytic Bone Metastasis Parenteral pamidronate/zoledronate
arrests osteolytic lesions and reduces bone pain.
Etidronate
This is the first BPN to be used clinically, employed in hypercalcaemia and Paget’s disease.
However, it also interferes with bone mineralization: continuous therapy
produces osteomalacia. Therefore, it has been largely replaced by zoledronate
for hypercalcaemia and alendronate/risedronate for Paget’s disease. Etidronate
is administered both orally and i.v., but is not preferred now. Adverse effects
are gastric irritation, bone pain, headache, metallic taste, pyrexia and
hypersensitivity.
Dose: 5–7.5 mg/kg/day; DRONATEOS 200 mg tab, 300 mg inj; DISONATE, ETIFEM 200 mg tab.
Pamidronate
A second generation potent BPN which is administered
only by i.v. infusion in a dose of 60–90 mg over 2–4 hours weekly or monthly
depending on the condition. It is used in Paget’s disease, hypercalcaemia of
malignancy and in bony metastasis. Adverse effects are thrombophlebitis of
injected vein, bone pain, fever and leukopenia. A fluelike reaction may occur
initially due to cytokine release.
AREDIA 15, 30, 60 mg
inj; AREDRONET 30, 90 mg inj.
BONAPAM 30, 60, 90 mg
ing.
Alendronate
This potent orally
effective second generation amino-BPN
is used primarily for prevention and treatment of osteoporosis both in women
and men. It is to be taken on empty stomach in the morning with a full glass of
water and patient is instructed not to lie down or take food for at least 30
min. These measures are needed to prevent contact with esophageal mucosa which
results in esophagitis. Calcium, iron, antacids, mineral water, tea, coffee,
fruit juice interfere with alendronate absorption. NSAIDs accentuate gastric
irritation caused by alendronate. Other adverse effects are gastric erosion,
retrosternal pain, flatulence, headache, bodyache and initial fall in serum
Ca2+ level.
Dose: 5–10 mg OD; or 35–70
mg weekly; weekly treatment is as
effective, more convenient and better tolerated. OSTEOPHOS, 5, 10, 35,
70 mg tab. DENFOS 5, 10 mg tab, RESTOFOS, DRONAL 10 mg tab.
Oral bioavailability of alendronate is ~1%. Up to 50% of the
drug entering the body is sequestrated in bone while the rest is excreted unchanged
mainly by the kidney. The terminal elimination t½ of alendronate has been
measured as 10.5 years.
Risedronate
It is an oral 3rd generation BPN, more potent than
alendronate, but equally efficacious. Oral bioavailability of 1% and other
features are also similar to alendronate. It is indicated in the treatment of
osteoporosis and Paget’s disease.
Dose: 35 mg/week oral in the
morning with a full glass of water.
RESTOFOS, GEMFOS,
ACTONEL 35 mg tab.
Zoledronate
This parenteral highly potent 3rd generation BPN is
indicated for hypercalcaemia, bony metastasis and Paget’s disease. Osteoclastic
activity is markedly suppressed and an additional antitumor effect may be
exerted by interference with mevalonate pathway. Proliferation of bony
metastasis of prostate/breast cancer and multiple myeloma cells may be
arrested. For hypercalcaemia, it is more effective, faster acting than
pamidronate and therefore the drug of choice now. Another advantage is that it
can be infused over 15 min (because of less venous irritation), whereas
pamidronate needs 2–4 hours. Fluelike symptoms due to cytokine release attend
the i.v. infusion. Renal toxicity has been encountered.
Dose: 4 mg diluted in 100 ml
saline/glucose solution and infused
i.v. over 15 min; may be repeated after 7 days and then at 3–4 week intervals.
ZOBONE, ZOLDRIA 4
mg/vial inj.
Related Topics
