Parathyroid Hormone
| Home | | Pharmacology |Chapter: Essential pharmacology : Drugs Affecting Calcium Balance
Vassale and Generali (1900) were the first to perform selective parathyroidectomy (without removing thyroids) and found that it produced tetany and death. MacCallum and Voegtlin in 1909 established this to be due to decrease in plasma calcium levels; parathormone (PTH) was isolated in 1925.
PARATHYROID HORMONE
(Parathormone)
Vassale and Generali (1900) were the first to perform selective
parathyroidectomy (without removing thyroids) and found that it produced tetany
and death. MacCallum and Voegtlin in 1909 established this to be due to
decrease in plasma calcium levels; parathormone (PTH) was isolated in 1925.
PTH is a single chain
84 amino acid polypeptide, MW 9500. It is synthesized as prepro-PTH, the excess
amino acids are split off in two steps and it is then stored in intracellular
vesicles. Secretion of PTH is regulated by plasma Ca2+ concentration through a
calcium-sensing receptor (CaSR), that is a G-protein coupled receptor on the
surface of parathyroid cells. There is no trophic hormone for it. Fall in plasma
Ca2+ induces PTH release and rise inhibits secretion by decreasing cAMP in the
parathyroid cells. Agents that increase cAMP cause PTH release, but direct
activation of protein kinase C by fall in Ca2+ concentration is more important
physiologically. Prolonged hypocalcaemia causes hypertrophy and hyperplasia of
parathyroids, while sustained hypercalcaemia has the opposite effect. Changes
in phosphate concentration in plasma affect PTH secretion indirectly by
altering Ca2+ concentration. The active form of vit. D calcitriol inhibits
expression of PTH gene in parathyroid cells. PTH is rapidly degraded in liver
and kidney; its plasma t½ is 2–5 min.
Actions
PTH increases plasma
calcium levels by:
Bone
PTH promptly increases resorption of calcium from bone.
This is the most prominent action of PTH—exerted by increasing the number of
bone remodeling units and activating osteoclasts when high concentrations are
present continuously. Since bone resorption is followed by new bone deposition,
this is also promoted by PTH: increased bone formation occurs when PTH is given
intermittently and in low doses.
Kidney
PTH increases calcium
reabsorption in the distal tubule
and provides moment to moment regulation of calcium excretion. It also promotes
phosphate excretion which tends to supplement the hypercalcaemic effect.
However, grossly increased plasma calcium level occurring in hyperparathyroidism
overrides the direct
action on tubules and
calcium excretion in urine is actually increased. The converse occurs in
hypoparathyroidism.
Intestines
PTH has no direct
effect on calcium absorption but
increases it indirectly by enhancing the formation of calcitriol (active form
of vit D) in the kidney by activating 1αhydroxylase.
Calcitriol then promotes intestinal absorption of calcium.
PTH decreases calcium
levels in milk, saliva and ocular lens—may be responsible for development of
cataract in hypoparathyroidism.
Mechanism Of Action
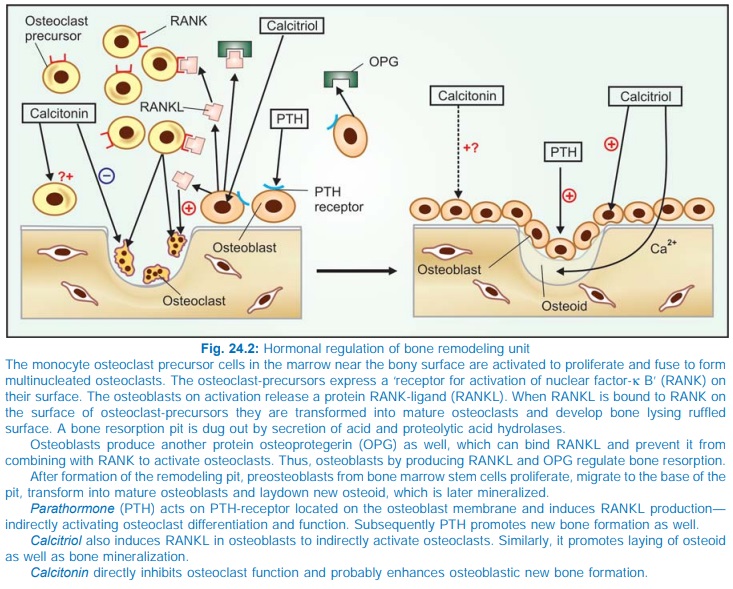
The PTH receptor is a G protein coupled receptor which on activation
increases cAMP formation and intracellular Ca2+ in target cells. In bone, the
target cell is the osteoblast because PTH receptors are not expressed on the surface
of osteoclasts. Acting on the osteoblast, PTH induces a factor ‘Receptor for
activation of nuclear facto-rκ-Bligand’ (RANKL) which diffuses and combines
with RANK on osteoclast precursors and transforms them into osteoclasts as well
as activates osteoclasts (Fig. 24.2). Moreover, birth rate of bone remodeling
units into which osteoclasts are recruited is enhanced. Formation of the
remodeling pit is followed by osteoblastic deposition of new bone into it. PTH
enhances proliferation and differentiation of preosteoblasts and deposition of
osteoid as well. Bone resorption predominates when high concentrations of PTH
are present continuously, but intermittent exposure to low concentrations has
the opposite effect.
Hypoparathyroidism
Manifestations are:
Low plasma calcium
levels, tetany, convulsions, laryngospasm, paresthesias, cataract and
psychiatric changes. Pseudohypoparathyroidism occurs due to reduced sensitivity
of target cells to PTH caused by a mutant G protein that couples PTH receptor
activation to cAMP generation in target cells.
Hyperparathyroidism
It is mostly due to parathyroid tumour. It produces—
Hypercalcaemia,
decalcification of bone—deformities and fractures (osteitis fibrosa
generalisata), metastatic calcification, renal stones, muscle weakness,
constipation and anorexia.
Treatment is surgical removal of
the parathyroid tumour. When this is not
possible—low calcium, high phosphate diet with plenty of fluids is advised.
Cinacalcet
It activates the Ca2+ sensing receptor (CaR) in the parathyroids and blocks PTH secretion. It
is indicated in secondary hyperparathyroidism due to renal disease and in
parathyroid tumour.
Use
PTH is not used in hypoparathyroidism
because plasma calcium can be
elevated and kept in the normal range more conveniently by vit D therapy. PTH
has to be given parenterally, while vit D can be given orally. Vit D is cheap.
However, recombinant human PTH (1–84 amino acid) has been produced and is being
clinically tested.
Teriparatide
This recombinant
preparation of 1–34 residues of amino
terminal of human PTH has been recently approved for the treatment of severe
osteoporosis. It duplicates all the actions of long (1–84) PTH. Injected s.c.
once daily, it has been found to increase bone mineral density in osteoporotic
women. The effect was faster and more marked than that produced by estrogens
and bisphosphonates (BPNs). Teriparatide is the only agent which stimulates
bone formation, whereas the other two only check bone resorption. In clinical
trials it was found to be equally or more effective than estrogens and BPNs in
reducing risk of vertebral as well as nonvertebral fractures. Its plasma t½ is
1 hr; given once daily only intermittent action is produced and bone forming
action predominates over bone resorbing action. High cost and need for daily
s.c. injections are the limitations.
Diagnostic use To differentiate pseudo from true hypoparathyroidism:
teriparatide is given i.v.: if plasma calcium level fails to rise, then it is
pseudohypoparathyroidism.
Related Topics
