Sedative -Hypnotics
| Home | | Pharmacology |Chapter: Essential pharmacology : Sedative -Hypnotics
A drug that subdues excitement and calms the subject without inducing sleep, though drowsiness may be produced. Sedation refers to decreased responsiveness to any level of stimulation; is associated with some decrease in motor activity and ideation.
SEDATIVE -HYPNOTICS
Sedative
A drug that subdues
excitement and calms the subject
without inducing sleep, though drowsiness may be produced. Sedation refers to
decreased responsiveness to any level of stimulation; is associated with some
decrease in motor activity and ideation.
Hypnotic
A drug that induces
and/or maintains sleep, similar to normal arousable sleep. This is not to be
confused with ‘hypnosis’ meaning a trans-like state in which the subject
becomes passive and highly suggestible.
The sedatives and
hypnotics are more or less general CNS depressants with somewhat differing time
action and dose action relationships. Those with quicker onset, shorter
duration and steeper dose-response curves are preferred as hypnotics while more slowly acting drugs with flatter dose-response curves are employed as sedatives. However, there is considerable overlap; a hypnotic at lower dose may act as
sedative. Thus, sedation—hypnosis—general anaesthesia may be regarded as
increasing grades of CNS depression. Hypnotics given in high doses can produce
general anaesthesia. However, benzodiazepines (BZDs) cannot be considered
nonselective or general CNS depressants like barbiturates and others.
Treatment of insomnia is the most important use of this class of
drugs.
Alcohol and opium have
been the oldest hypnotics and continue to be used for this purpose as self-medication
by people. Bromides introduced in 1857 are now obsolete, so are chloral hydrate
(1869) and paraldehyde (1882). Fischer and von Mering introduced barbitone in
1903 and phenobarbitone in 1912. Barbiturates reigned supreme till 1960s when
benzodiazepines started eroding their position and have now totally replaced
them. In the mean time, a number of other sedative-hypnotics were introduced but
none was significantly different from barbiturates; all are redundant now. Some
new non-BZD hypnotics have become available over the past decade.
Sleep
The duration and
pattern of sleep varies considerably among individuals. Age has an important effect
on quantity and depth of sleep. It has been recognized that sleep is an
architectured cyclic process (Fig. 29.1). The different phases of sleep and
their characteristics are—
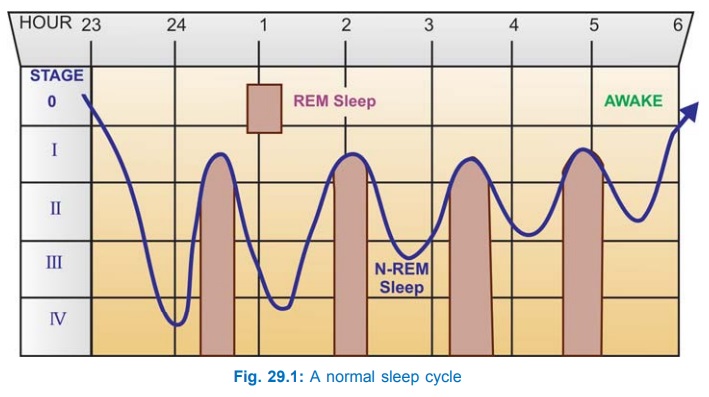
Stage 0 (awake) From lying down to
falling asleep and occasional nocturnal awakenings;
constitutes 1–2% of sleep time. EEG shows α activity when eyes
are closed and β activity when eyes are open. Eye movements are irregular or
slowly rolling.
Stage 1 (dozing) α activity is interspersed
with θ waves. Eye movements are reduced but there may be
bursts of rolling. Neck muscles relax. Occupies 3–6% of sleep time.
Stage 2 (unequivocal sleep) θ waves with
interspersed spindles, K complexes
can be evoked on sensory stimulation; little eye movement; subjects are easily
arousable. This comprises 40–50% of sleep time.
Stage 3 (deep sleep transition) EEG shows θ, δ and spindle activity, K complexes can be evoked
with strong stimuli only. Eye movements are few; subjects are not easily
arousable; comprises 5–8% of sleep time.
Stage 4 (cerebral sleep) δ activity predominates
in EEG, K complexes cannot be
evoked. Eyes are practically fixed; subjects are difficult to arouse. Night
terror may occur at this time. It comprises 10–20% of sleep time.
During stage 2, 3 and 4 heart rate, BP and respiration are
steady and muscles are relaxed. Stages 3 and 4 together are called slow wave
sleep (SWS).
REM sleep (paradoxical sleep) EEG has waves of all frequency, K complexes cannot be elicited.
There are marked, irregular and darting eye movements; dreams and nightmares
occur, which may be recalled if the subject is aroused. Heart rate and BP
fluctuate; respiration is irregular. Muscles are fully relaxed, but irregular
body movements occur occasionally. Erection occurs in males. About 20–30% of
sleep time is spent in REM.
Normally stages 0 to 4 and REM occur in succession over a period
of 80–100 min. Then stages 1–4–REM are repeated cyclically.
The EEG waves have
been divided into—
α: high amplitude, 8–14 c.p.s. (cycles per second)
β: low amplitude, 15–35
c.p.s.
θ: low amplitude, 4–7 c.p.s.
δ: high amplitude, 0.5–3 c.p.s.
K complex: deep
negative wave followed by positive wave and a few spindles.
Classification
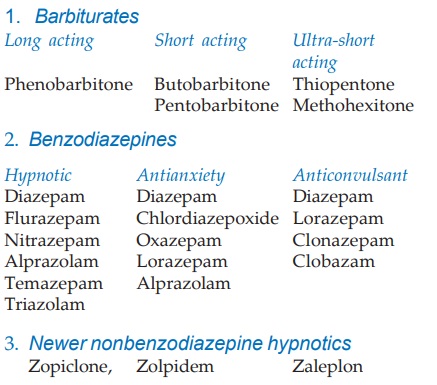
Chloral hydrate,
Triclophos, Paraldehyde, Glutethimide, Methylprilone, Methaqualone and
Meprobamate are historical sedative hypnotics no longer used. They are
described in earlier editions of this book.
In addition some
antihistaminics (promethazine, diphenhydramine), some
neuroleptic/antidepressants (chlorpromazine, amitriptyline), some
anticholinergic (hyoscine) and opioids (morphine, pethidine) have significant
sedative action, but are not reliable for treatment of insomnia.
