Small Intestine
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Digestive System
Extending from the pyloric sphincter to the large intestine, the small intestine is a tubular organ with many loops and coils filling much of the abdominal cavity.
Small
Intestine
Extending from the pyloric sphincter to the large intestine,
the small intestine is a tubular
organ with many loops and coils filling much of the abdominal cavity. It
receives secretions from the liver and pancreas, completing digestion of the
nutrients in chyme. It also absorbs the products of digestion and transports
the remaining residues to the large intes-tine. The small intestine is the
longest portion of the alimentary canal, yet its diameter is only about half
that of the large intestine. It is approximately 6–7 m or about 20 feet in
length but only about 2.5–4 cm or 1–1.6 inches in diameter. Because of loss of
muscle tone, the small intestine is smaller in a cadaver, only 2–4 m or 7–13
feet.
The small intestine plays the major role in the diges-tion and absorption of nutrients, with
90% of nutrient absorption occurring there. Most of the remaining absorption of
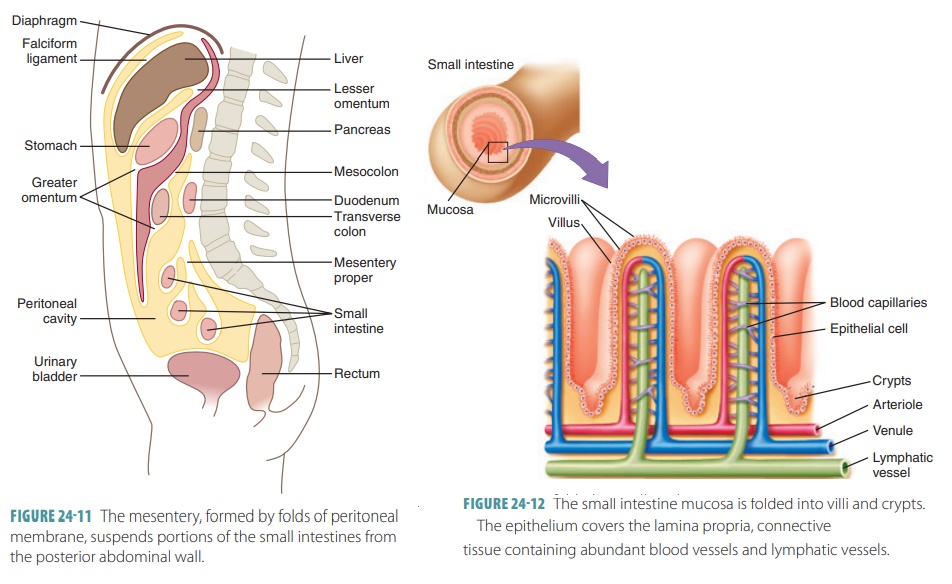
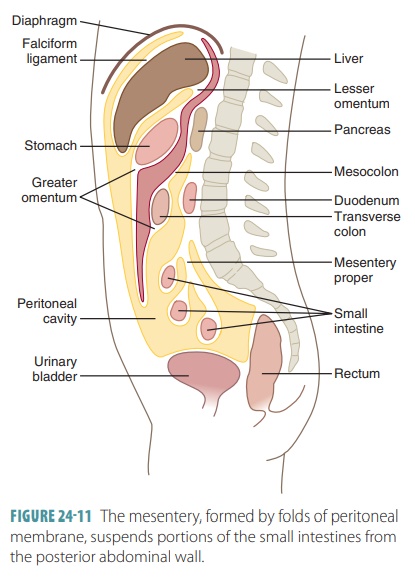
nutrients occurs in the large intestine. The small intestine consists of three
portions: duodenum, jejunum, and ileum (FIGURE 24-10). The duodenum is mostly
retroperitoneal, whereas the other portions are intraperitoneal. The lining of
the small intestine has approximately 800 transverse folds known as plicae circulares. They do not disappear when the small intes-tine is
filled, unlike the rugae of the stomach. The plicae circulares increase the
absorptive surface area of the small intestine.
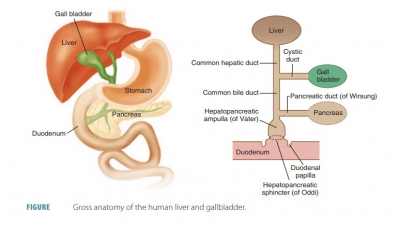
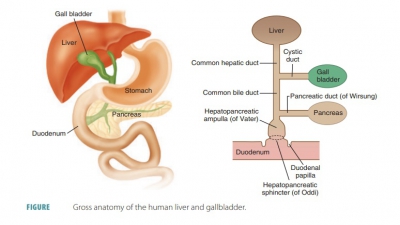
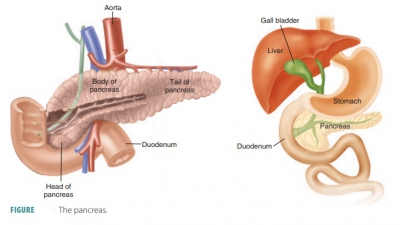
The duodenum is about 25 cm or 10 inches long and 5 cm or 2 inches in diameter and relatively immovable. It is located posterior to the parietal peritoneum, following a C-shaped path by passing anterior to the right kidney and upper three lumbar vertebrae. The duodenum is curved around the head of the pancreas. It functions as a mixing area, receiv-ing chyme from the stomach and digestive secre-tions from the pancreas and liver. The duodenum is the shortest portion of the small intestine yet has the most interesting functions. The bile duct delivers bile from the liver. The main pancreatic duct brings pancreatic juice from the pancreas. These ducts unite in the duodenal wall at the hepatopancreatic ampulla, which resembles a bulb and opens into the duodenum through the major duodenal papilla. The hepatopancreatic sphincter is a smooth muscle valve that controls entry of the substances from the liver and pancreas. The remainder of the small intestine is more mobile, lying free inside the peritoneal cavity.
The jejunum is the
proximal two-fifths of the small intestine and is about 2.5 m or 8 feet in
length and about 4 cm or about 1.5 inches in diameter. It links the duodenum
with the ileum. Most chemical diges-tion and nutrient absorption occur in the
jejunum. The jejunum, along with the next segment, appears like coiled sausage
in the central, lower abdominal cavity.
The final segment of the small intestine is called the ileum, which is not distinctly separate from the jejunum but has
a smaller diameter, with a thinner, less vascular, and less active wall. It is
the longest portion of the small intestine, totaling about 3.6 m or 12 feet in
length. The ileum ends at the ileocecal
valve, which controls the flow of substances from the ileum into
the large intestine.
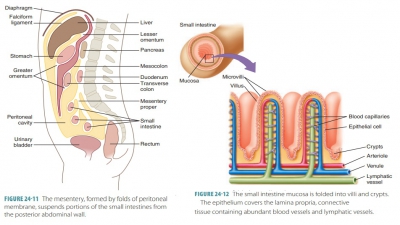
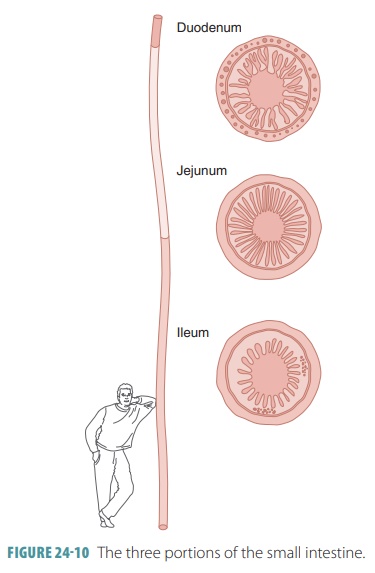
The mesentery is a
double-layered fold of peritoneal membrane that suspends the jejunum and ileum
from the posterior abdominal wall (FIGURE
24-11). The mesentery supports the blood vessels, lymphatic vessels,
and nerves that supply the intestinal wall. A double fold of peritoneal
mem-brane called the greater omentum
drapes from the stomach over the transverse colon and folds of the small
intestine. If the alimentary canal walls become infected, the greater omentum’s
cells may adhere to the inflamed area, helping to prevent the infection from
spreading to the peritoneal cavity.
The small intestine is served by parasympathetic nerve
fibers from the vagus nerve and sympathetic nerve fibers from the thoracic splanchnic
nerves. Both types are relayed via the superior mesenteric and celiac plexuses.
Arterial blood is supplied mostly from the superior mesenteric artery. The
similarly routed veins mostly drain into the superior mesenteric vein.
Nutrient-rich blood from the small intestine drains through these veins to the
hepatic portal vein, and is then carried to the liver.
Microscopic Structures of the Small Intestine
The length of the small intestine provides a large sur-face
area for absorbing nutrients. This is increased by more than 600 times by the
presence of its circular folds, villi, and microvilli. These specialized
structures are more numerous near the distal small intestine, so it is here
where most absorption occurs. The total intestinal surface area of the small
intestine is approx-imately 200 square meters.
The small intestine’s circular folds (plicae circu-laris) of the mucosa
and submucosa are deep and do not change. Each fold is about 1 cm or about 4/10
inch in height and functions to force chyme into a spiral-ing movement through
the lumen of the small intes-tine. This slows down its movement, so full
nutrient absorption has time to occur.
The inner wall of the small intestine has many tiny
finger-like projections of the mucous membrane called intestinal villi (FIGURE 24-12). The villi are slightly more than 1 mm or about 4/100 inch
in length and give the inner wall a soft texture similar to vel-vet fabric.
They are most numerous in the duodenum and proximal jejunum, decreasing in size
along the way from the duodenum to the ileum. The villi help to contract the
intestinal contents and increase the sur-face area of the intestinal lining to
aid in absorption of digestive products. In the duodenum, the villi appear like
leaves.
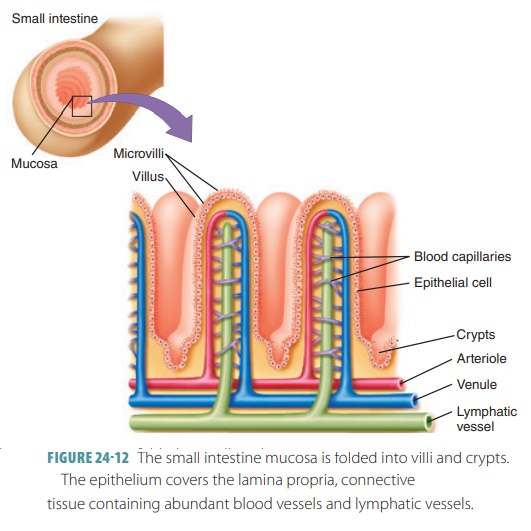
Each villus has a layer of absorptive, simple columnar
epithelium consisting of enterocytes,
a core of connective tissue with capillaries, a lymphatic cap-illary called a lacteal, and nerve fibers. The cores have
dense capillary beds. The lacteals are actually wide lymphatic capillaries.
Nutrients are carried away by blood capillaries and lacteals. Extremely long
and densely packed microvilli are
found in the absorptive mucosal cells. Therefore, the mucosal surface appears
“fuzzy” and is referred to as the brush
border.
In the small intestine, the major mixing move-ment is
segmentation, meaning small, ring-like con-tractions occur periodically to cut
the chyme into segments and move it back and forth. This slows its movement
through the small intestine. These weak peristaltic waves result in chyme
taking between three and 10 hours to move through the small intestine.
Overdistention or irritation of the small intestine results in a peristaltic rush, which moves the small intestine’s contents into the large intestine quickly. Normal absorption of nutrients, water, and electro-lytes, therefore, does not occur in this situation. Peri-staltic rush results in diarrhea, and prolonged diarrhea results in water and electrolyte imbalances.
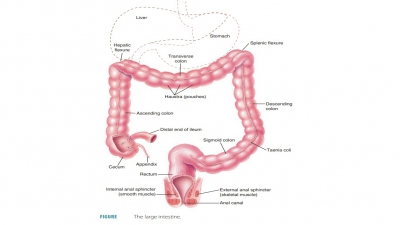
The small intestine connects to the large intes-tine via a
valve called the ileocecal
sphincter. This sphincter is usually constricted to keep the contents
of each intestine separate. After eating, peristalsis in the ileum relaxes the
sphincter to force some small intes-tine contents into the cecum of the large intestine.
Intestinal Glands
Intestinal
glands are located between the bases of adjacent villi and extend downward into the
mucous membrane. There are five types of cells in the mucosal epithelium:
■■ Enterocytes:
These make up most of the epithelium, and are simple, columnar absorptive
cells. The enterocytes are bound with tight junctions and have many microvilli.
They are mostly responsible for absorption of nutrients and electrolytes within
the villi. Inside the crypts, they are the main cells that secrete intestinal
juice, which is watery and contains mucus. This juice carries absorbing
nutrients from the chyme.
■■ Goblet
cells: Which secrete mucus, exist through out the mucosa of the small
intestine, in its villiand crypts. Specialized mucous-secreting glands in the
proximal duodenum secrete thick, alkaline mucus when specifically stimulated to
do so. At the bases of the villi, intestinal glands secrete high volumes of a
watery fluid with a nearly neutral pH. This fluid lacks digestive enzymes. The
enzymes in the luminal surfaces of the intestinal mucosa break down food just
before absorption. These enzymes include pep-tidases, sucrose, maltase,
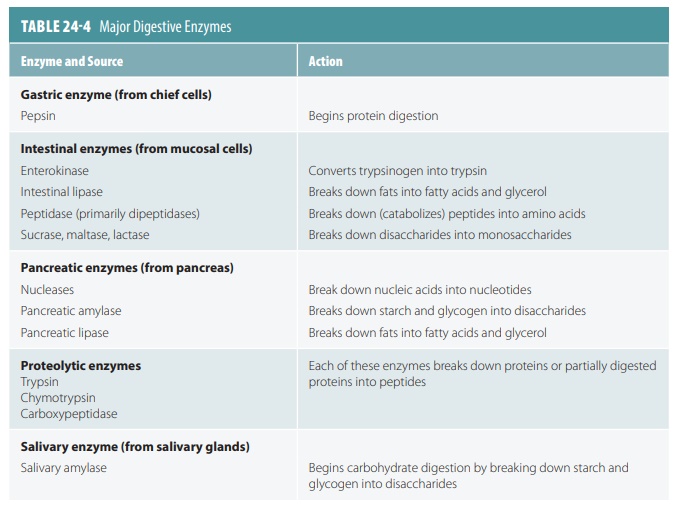
lactase, and intestinal lipase. TABLE
24-4 summarizes these enzymes, their sources, and their actions.
When stimu-lated by chyme, goblet cells and intestinal glands secrete their
products. As the intestinal wall dis-tends, it activates nerve plexuses,
stimulating parasympathetic reflexes that trigger release of small intestine
secretions.
■■ Enteroendocrine
cells: The source of enterogas-trones such as secretin and cholecystokinin.
They are mostly presented throughout the crypts, but are found in lesser
numbers in the villi.
■■ Paneth
cells: Existing deep inside the crypts, these specialized secretory cells strengthen the defenses of the small
intestine by releasing defensins, lysozyme, and other antimicrobial agents.
Their secretions destroy various bacteria and aid in the determination of which
bacteria form colonies within the intestinal lumen.
■■ Stem cells: Continuously dividing deep in the crypts, their daughter cells differentiate into all other types of cells. Most daughter cells, except for Paneth cells, differentiate while migrating up the villi. The Paneth cells migrate to the bottoms of the crypts. At the tips of the villi, epithelial cells undergo apoptosis. They are shed, and the villus epithelium is renewed every three to five days.
Intestinal Juice
Nearly 1–2 liters or about 1–2 quarts of intestinal juice
are secreted by the intestinal glands every day. Hyper-tonic or acidic chyme is
the major causative factor for this secretion because it causes the intestinal
mucosa to be distended or irritated. In normal conditions, the intestinal juice
is isotonic with the blood plasma and slightly alkaline, between 7.4 and 7.8
pH. Although mostly made of water, it also contains mucus secreted by the
duodenal glands and mucosal goblet cells. Intestinal juice does not have high
enzyme content because intestinal enzymes are mostly found at the brush border.
1. Explain the actions of the circular folds, villi,
microvilli, and brush border.
2. What is the importance of the mesenteries?
3. Describe the three portions of the small intestine.
4. What are the five types of cells in the mucosal epithelium
of the small intestine?