Stomach
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Digestive System
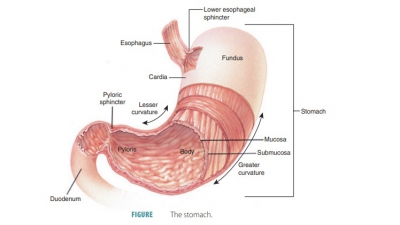
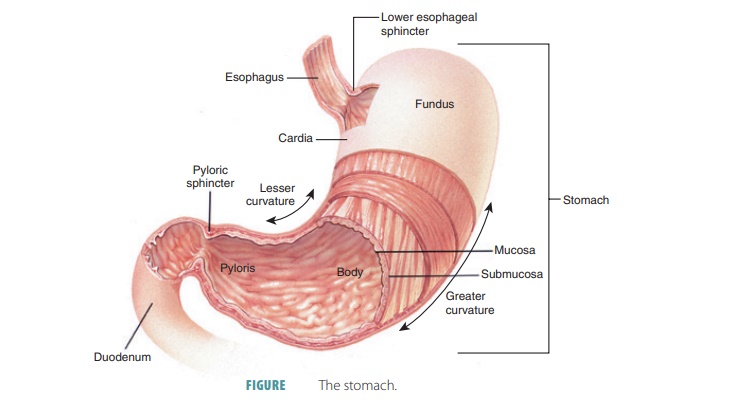
The stomach is a pouch-like organ shaped like the letter “J.”
Stomach
The stomach is a
pouch-like organ shaped like the letter “J.” It hangs inferior to the
diaphragm, in the upper left abdominal cavity, and is partially obscured by the
liver and diaphragm. The stomach is approximately 15–25 cm or 6–10 inches in
length, although its volume and diameter change based on how much food is
contained. When empty, its volume is about 50 mL, and it has a cross-sectional
diameter just a little larger than the large intestine. The organ collapses
inward when empty. Its capacity is approx-imately 4 liters or 1 gallon, and its
inner lining con-sists of thick folds of mucosal and submucosal layers called rugae. When the stomach is distended, these folds disappear, and
it can extend downward almost to the pelvis. The stomach is very movable in its
mid-dle regions but fixed at either end. The stomach mixes food from the
esophagus with gastric juice, begins protein digestion and limited absorption,
and moves food into the small intestine (FIGURE 24-8). It is divided into the cardiac, fundic, body, and pyloric
regions:
■■ Cardiac
region: A small area near the esophageal
opening. This portion of the stomach that attaches to the esophagus is
called the cardia or cardial part. It surrounds the cardial
orifice, which is where food enters
from the esophagus.
■■ Fundic
region: Balloons superior to the cardiac
portion and acts as a temporary storage area. It is also called the fundus and is dome-shaped. The fundus is
located beneath the diaphragm. It bulges superolaterally to the cardia.
■■ Body
region: The dilated, main portion of the
stomach. It is the large middle portion, commonly called the body, and is continuous inferiorly with
the pyloric region.
■■ Pyloric
region: Narrower than the rest of the
stomach, this funnel-shaped region begins with a wider and superior pyloric antrum, becoming the pyloric canal as it nears the small intestine. This terminates at
the pylorus. At its end, the muscular wall thickens to form a powerful,
circu-lar pyloric sphincter, which
acts as a valve con-trolling gastric emptying. The pylorus is actually
continuous with the duodenum.
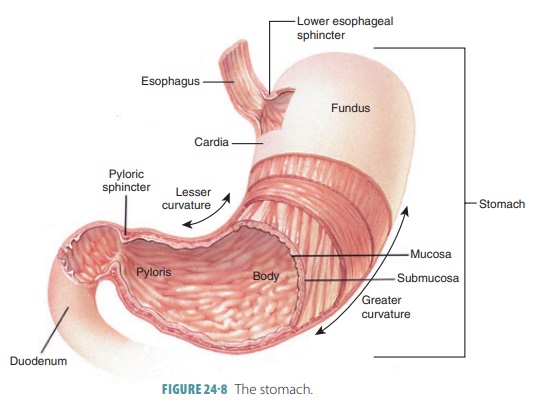
The greater
curvature of the stomach is its con-vex lateral surface. The
stomach’s lesser curvature is its
concave medial surface. Two mesenteries extend from these curvatures. Known as omenta, they help tie the stomach to the body wall and other
digestive organs. The two omenta are individually named the lesser omentum and
the greater omentum.
The lesser omentum links the lesser curvature of the stomach
to the liver. It is continuous with the visceral peritoneum that covers the
stomach. The greater omen-tum is draped inferiorly from the greater curvature,
cov-ering the small intestine’s coiled structure. It continues dorsally and
superiorly to wrap the spleen and trans-verse large intestine. Then, it blends
with the mesocolon, which is a dorsal
mesentery securing the large intestine to the parietal peritoneum of the
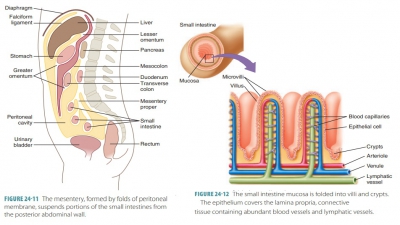
posterior abdominal wall. The mesentery
proper is a thick sheet that suspends all the small intestine, except for
the first 25 cm or 10 inches. It allows movement yet provides stability.
The autonomic nervous system serves the stom-ach. Thoracic
splanchnic nerves relay sympathetic fibers through the celiac plexus. The vagus
nerve sup-plies parasympathetic fibers. The gastric and splenic branches of the
splenic trunk provide the stomach’s arterial supply. Its corresponding veins
are part of the hepatic portal system. They eventually drain into the hepatic
portal vein.
Microscopic Anatomy of the Stomach
Like most of the alimentary canal, the wall of the stom-ach
contains four tunics. However, its muscularis and mucosa have specialized
functions. The muscularis externa has an incomplete, innermost, smooth muscle
fibril layer, which runs obliquely. This is in addition to the usual
longitudinal and circular layers of smooth muscle of the rest of the alimentary
canal.
The stomach mucosa has a simple columnar epi-thelium made up
only of mucous cells. A two-layer coat of cloudy alkaline mucus protects the
stomach. The top layer of mucus is viscous and insoluble. It keeps the second
layer trapped beneath it, which consists of rich amounts of bicarbonate. The
stomach’s inner lining of mucous membranes is thick, with many small gastric pits at the ends of tubular gastric glands. These glands have three main types of secretory cells:
mucous, chief, and parietal cells. Mucous cells lie in the necks of the glands
near the gastric pit openings; chief and parietal cells are in the deeper
areas. The gastric pits have walls that are mostly formed by mucous cells.
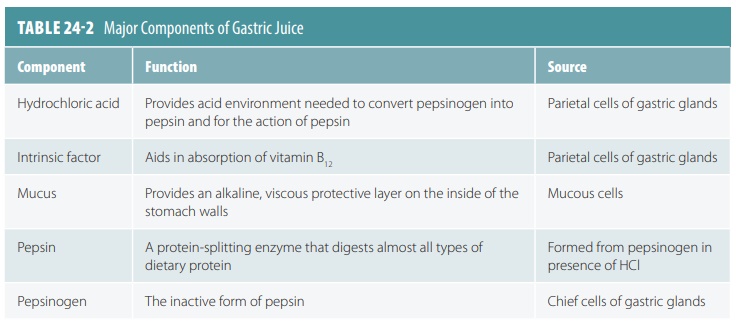
Together, the three types of secretory cells produce gastric juice. Mucus is secreted
primarily from the cells in the glands of the cardia and pylorus. In the
pyloric antrum, the cells produce mucus as well as several hormones, which
include most of the gastrin, a stimulatory hormone. Gastric juice denatures
proteins and inactivates most enzymes found in food. Gastric juice components
are summarized in TABLE
24-2.
Types of Gland Cells
The glands of the fundus and body are much larger than in
other areas and produce most of the secre-tions from the stomach. Most
digestion occurs in these areas. The glands here contain many different
secretory cells, which include mucous neck, parietal, chief, and
enteroendocrine cells. The mucous neck
cells are located in the neck and
more basal regions of the stomach
glands. They produce a thinner, more soluble mucus than the mucous cells of the
surface epithelium. This acidic mucus is not fully understood in its function
but helps to prevent the stomach from digesting itself.
Parietal Cells
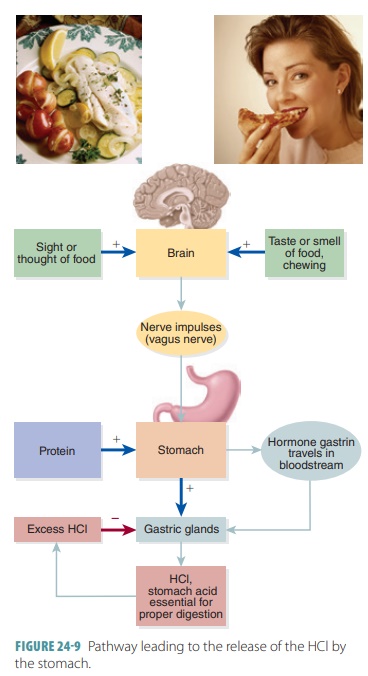
The parietal
cells are found mostly in the more apical region of stomach
glands and are scattered among the chief cells. The parietal cells secrete both
hydrochloric acid (HCl) and the glycoprotein known as intrinsic factor. HCl causes the contents of the stomach to be very acidic, with a pH between 1.5 and
3.5, a condition needed so pepsin can be
activated effectively. HCl, and the environment it creates, is able to denature
pro-teins, break down plant food cell walls, break down connective tissues from
meats, and kill most bacteria ingested with foods and is of significant
importance for digestion. For vitamin B12 to be absorbed in the
small intestine, intrinsic factor is required. Negative feedback is used to
regulate the concentration of HCl in the stomach (FIGURE 24-9).
Chief Cells
Chief
cells are most abundant near the base of a gas-tric
gland. Cuboidal chief cells secrete pepsinogen,
an inactive proenzyme that is converted by the acid in the gastric lumen to
pepsin, an active proteolytic or protein-digesting enzyme. Stimulation of
these cells results in the
first-released pepsinogen molecules to be activated by HCl in the apical region
of the gland. When pepsin becomes present, it additionally cata-lyzes
pepsinogen conversion into more pepsin. This activation requires a small
fragment of peptide from pepsinogen. When the fragment is removed, the
pep-sinogen changes shape and its active site is exposed. This is a positive
feedback process that is unlimited, except for the amount of available
pepsinogen. The chief cells also secrete fat-digesting enzymes known as
lipases, which are believed to handle nearly 15% of all lipolysis in the
gastrointestinal tract.
Enteroendocrine Cells
Enteroendocrine
cells release many chemical mes-sengers into the
interstitial fluid of the lamina propria. They are usually found deep inside
gastric glands. Some act locally as paracrines such as serotonin and histamine. Somatostatin and other messengers act locally as paracrines and also as hormones,
which diffuse into blood capillaries, influencing several digestive system
target organs. Gastrin
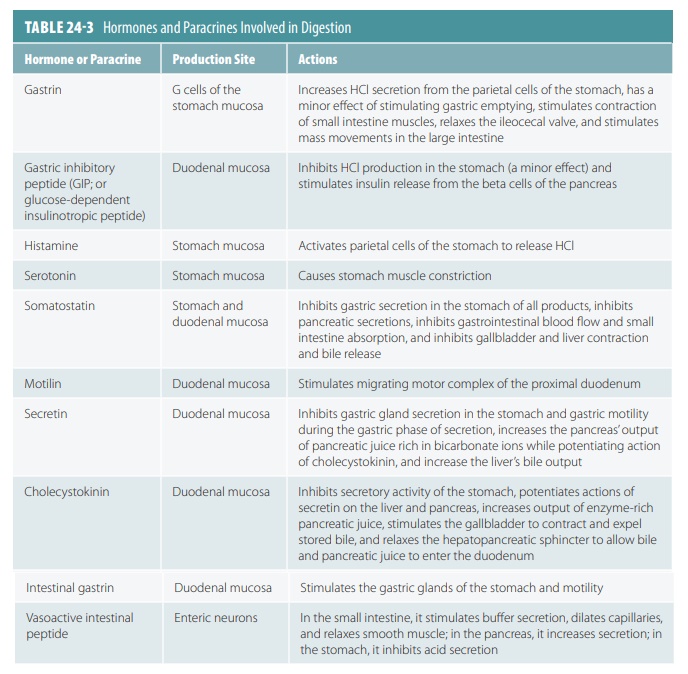
is one of the hormones vital for regulating stomach secretion and motility. TABLE 24- 3 explains the hormones
and para-crines involved in digestion.
Mucosal Barrier
The mucosal
barrier is responsible for the stomach’s self-protection against
corrosive and acidic gastric juices. Protein-digesting enzymes in this juice
are able to actually digest the stomach. For example, the hydrogen ion
concentration of the stomach can be up to 100,000 times of the same
concentration that is in the blood. The mucosal barrier is created by the
fol-lowing three factors:
■■ Mucus:
A thick coating, built up on the stomach walls, which is rich in bicarbonate.
■■ Tight
junctions: The mucosa’s epithelial cells are joined tightly together,
preventing gastric juice from leaking into tissue layers that lie underneath .
■■ Cell
replacement: Damaged epithelial mucosal
cells are shed, then quickly replaced as undiffer-entiated stem cells
divide; these cells lie in areas where gastric pits join gastric glands. The
surface epithelial mucosal cells are totally renewed every three to six days.
However, deeper and better- protected glandular cells inside the gastric
glands live for a much longer period of time.
Digestion in the Stomach
The stomach not only holds ingested foods, but also
physically and chemically degrades them, which produces chyme. Chyme is then moved from the stomach to the small intestine. The
primary type of enzymatic breakdown in the stomach is pro-tein digestion. HCl
denatures dietary proteins so enzymes can digest them. The amino acid chains in
dietary proteins are unfolded, so digestive enzymes become more effective.
Pepsin is the most important protein-digesting enzyme
produced by the gastric mucosa, but in infants, rennin is another stomach enzyme that is needed. Rennin converts
milk protein or casein into a
curd-like substance. Lingual lipase from salivary glands also helps to digest
certain triglycerides in the stomach, until the lipase also becomes digested.
Lipid-soluble substances, such as aspirin or alcohol, easily pass through the
mucosa of the stomach into the blood. Both of these substances are prone to
caus-ing gastric bleeding and should not be used if a gastric ulcer is present.
However, the secretion of intrinsic factor is actually the
only stomach function that is essential
for life. Intrinsic factor is vital
for the intestine to absorb vitamin B12, which is required for
production of mature erythrocytes. Without this, pernicious ane-mia develops. Even after a complete surgical removal of the stomach, known as a total gastrectomy, injected vitamin B12
minimizes digestive problems.
1. List and name the various portions of the stomach.
2. What are pepsin and pepsinogen and the substances needed
for their production?
3. Which types of stomach epithelial cells secrete pepsin and
pepsinogen?
4. Explain how the mucosal barrier of the stomach is created.
Gastric Secretion
Gastric secretion is controlled by neural and hor-monal
mechanisms. Normally, about 3 liters of gas-tric juice are released by the
gastric mucosa every day. This acidic mixture is so strong it can dissolve metal
objects. Nervous control of gastric secretion is pro-vided by long and short
nerve reflexes. Long reflexes are mediated by the vagus nerve and short
reflexes are local, enteric reflexes. Nearly all stomach glands expe-rience
increased secretory action when the stomach is stimulated by the vagus nerve.
Secretory activity is reduced by activation of the sympathetic nerves.
Gastrin is the primary hormonal controller of gastric
secretion. It stimulates secretion of both HCl and enzymes. Small intestine hormones
also help to control gastric secretion and are primarily gastrin antagonists.
The three phases of gastric secretion are the cephalic, gastric, and intestinal
phases. For all these, the stomach acts as the effector site. Once begun,
one or all phases may occur simultaneously.
Cephalic (Reflex) Phase
The cephalic
(reflex) phase is the first to occur, hap-pening before food enters the
stomach. It lasts for a few minutes and is triggered by the smell, sight,
taste, or even thought of food. This phase prepares the stom-ach for digestion
via the vagus nerve.
Gastric Phase
When food enters the stomach, the gastric phase is started by local neural and
hormonal processes. The gastric phase lasts for three to four hours. About
two-thirds of the gastric juice that is released is provided by this phase.
Protein- rich foods in the stomach cause the pH to usually rise because
proteins buffer hydro-gen ions. The higher pH stimulates gastrin secretion,
then the release of HCl. This provides the required amount of acid needed to
digest the proteins. Higher amounts of proteins in food cause more gastric
juice and HCl to be released. During digestion, the gastric contents eventually
become more acidic. This inhibits the gastrin-secreting cells once again, a
negative feed-back mechanism that maintains desired pH needed for gastric
enzymes to work. Besides gastrin, ace-tylcholine and histamine also stimulate
this phase. When just one of these three chemicals binds to parietal cells,
secretion of HCl is minimal. When all three of them bind, however, HCl
secretion is exten-sive. Histamine is most critical in this regard, and
therefore antihistamines such as cimetidine are used to treat gastric ulcers
caused by hyperacidity. This is because they bind to and block the histamine recep-tors
of the parietal cells.
Intestinal Phase
There are both stimulatory and inhibitory compo-nents of the
intestinal phase. As
partly digested foods fill the duodenum of the small intestine, the excitatory
or stimulatory actions begin. The
intesti-nal mucosal cells are stimulated to release intestinal or enteric
gastrin. This hormone keeps the gastric glands continually
secreting. However, the effect is short as the intestine is distended with
chyme that has many fats, hydrogen ions, partially digested proteins, and
various irritants. The enterogastric
reflex then triggers the inhibitory actions.
The enterogastric reflex is made up of three actions: inhibition of the vagal nuclei in the medulla oblongata, inhibition of local reflexes, and activation of sympathetic fibers, causing tightening of the pyloric sphincter. This tightening prevents additional entry of food into the small intestine. Several intestinal hor-mones called enterogastrones are then released, which include secretin, cholecystokinin, and vasoactive intestinal peptide (VIP). They inhibit gastric secretion while the stomach is highly active and play various other roles.
1. Explain the most important substances required for normal
digestion.
2. What are the three phases of gastric secretion?
3. Describe how eating a large meal, in comparison with a smaller one, affects stomach emptying.