Spectrum of Activity of Chemotherapeutic Agents
| Home | | Medicinal Chemistry |Chapter: Medicinal Chemistry : History and Development of Chemotherapy
The ability of drug with all ranges (gram positive and gram negative) of antibiotic action, chloramphenicol, and tetracycline, to antagonize numerous pathogens have resulted mention as broad-spectrum antibiotics.
SPECTRUM OF ACTIVITY OF CHEMOTHERAPEUTIC AGENTS
The ability
of drug with all ranges (gram positive and gram negative) of antibiotic action,
chloramphenicol, and tetracycline, to antagonize numerous pathogens have
resulted mention as broad-spectrum antibiotics. Many of the broad-spectrum
antibiotics are active only at high concentration. Some drugs are primarily
static and they may exert cidal action at high concentration (e.g.
sulphonamides, erythromycin, nitrofurantoin, etc). The bacteriostatic agents
are those that interfere with the growth or replication of microorganisms, but
does not kill it. The bactericidal drugs are those that kills the
microorganisms. Concentration of drugs at the site of infection is an important
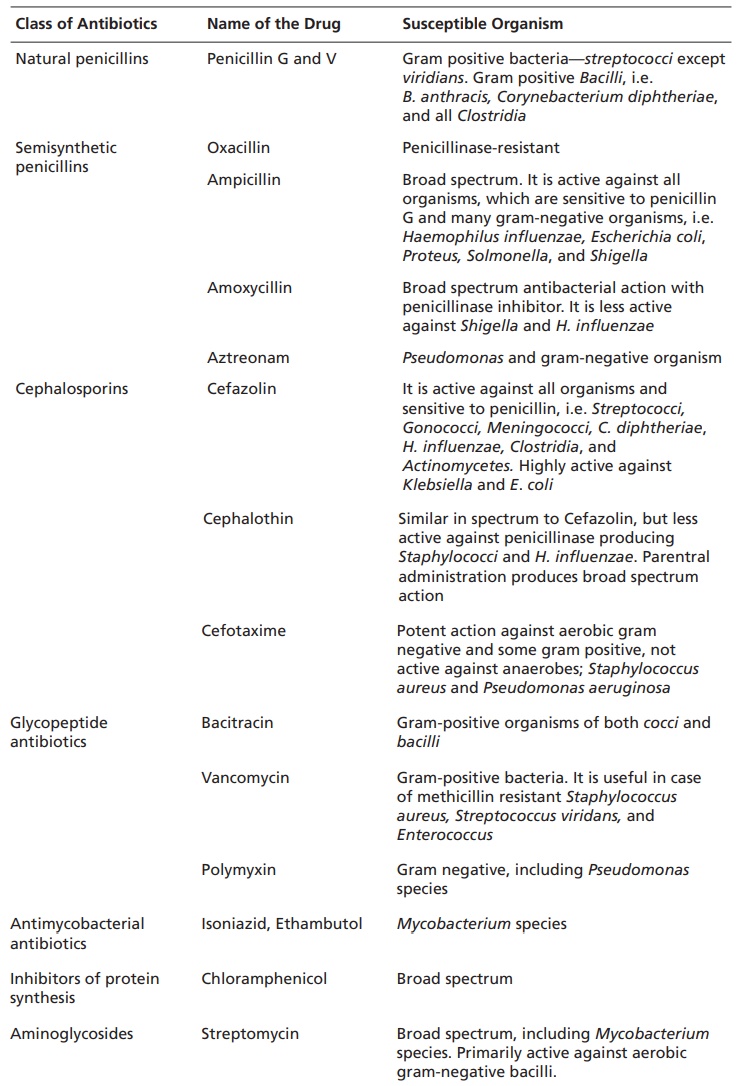
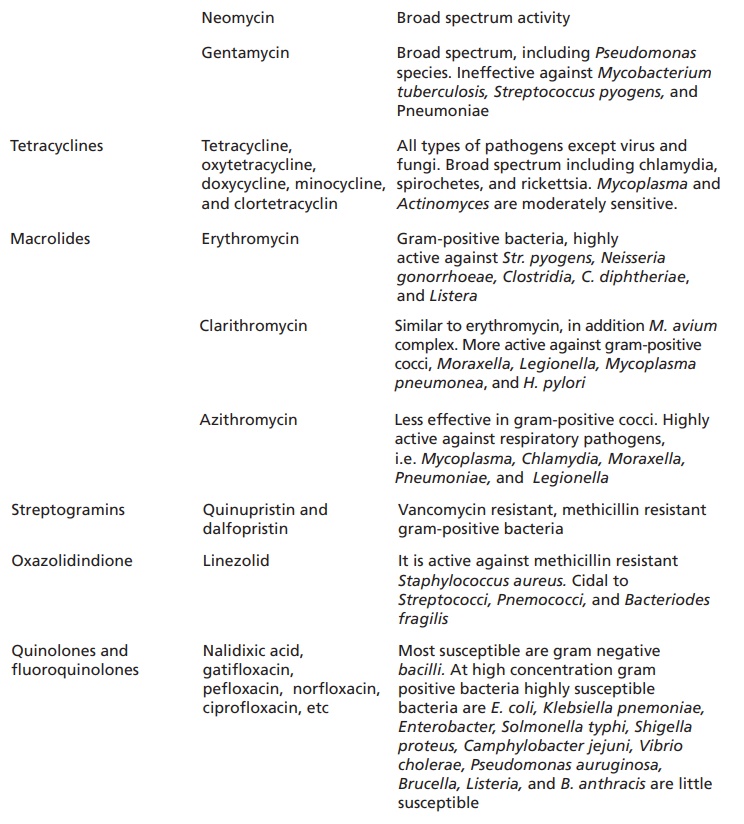
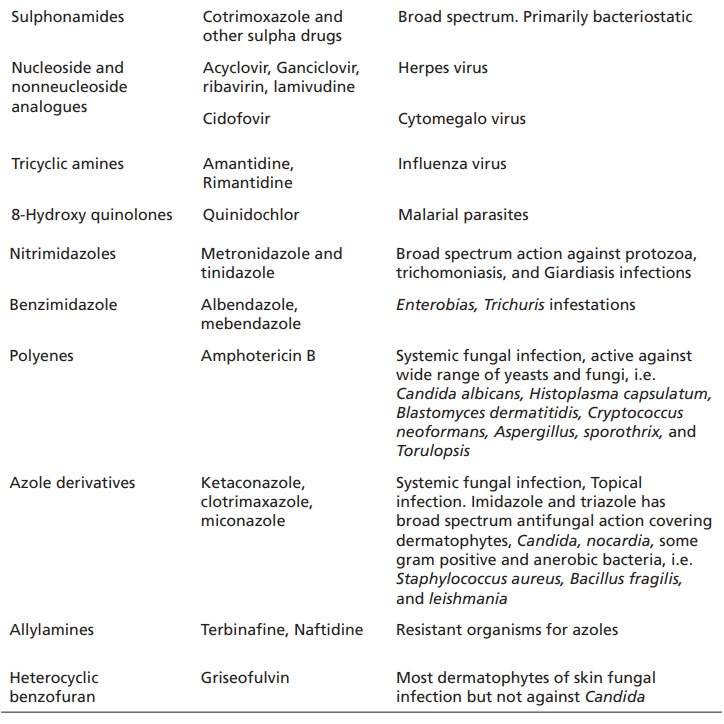
factor for the therapeutic effect in case of antimicrobials. The classes of
antibiotics and their spectrum of activity is detailed in Table 1.1.
Table 1.1 Classes of antibiotics and their spectrum of activity.
Bacterial Resistance to Antimicrobial Agents
The
bacterial resistance development depends on three factors. They are as follows:
·The necessary dose or concentration not reached
to target.
·The chemotherapeutic agent is not active.
·The target is altered.
The outer
membrane of the gram-negative bacteria is a permeability barrier that excludes
large polar molecules, including antibiotic, through a protein called porins.
Loss of porin channel may prevent the entry of antibiotics and reduces the
concentration in target site. If there is an active transport mechanism for the
entry of drug into the cell, mutational changes will occur in the transport to
produce resistant. For example, passage of gentamycin across the microbial cell
membrane by concentration gradient by involving the respiratory electron
transport and oxidative phosphorylation. Mutation in this enzyme pathway
decreases the concentration to the target.
Inactivation
of drugs are seen in case of aminoglycoside and β-lactums. In aminoglycosides,
the acquisition of cell membrane bound inactivating enzymes which
phosphorylates/adenylates or acetylates the drug molecule and produces
conjugated aminoglycosides. These conjugated amino glycosides do not bind to
target ribosome and so are incapable of enhancing active transport. Nosocomial
microbes have rich plasmids producing multidrug resistance and cross
resistance.
In
fluroquinolone, the resistance is occurred by alteration of target. The
resistance is noted due to chromosomal mutations producing a DNA gyrase or
topoisomerase IV with reduced affinity to the fluroquinolone or due to reduced
permeability of the drug.
Selection of Antimicrobial Agents
The
selection is based on thorough knowledge of pharmacological and microbiological
factors. Antibiotics are used in three general ways such as empirical therapy,
definitive therapy, and prophylactic therapy. When used in empirical, the drug
intended should cover all the microorganisms, if the pathogen is exactly not
known. In the combination therapy,
treatment with a broad spectrum antibiotic is necessary. After the
identification of infecting microorganism, selective drug can be used.
COMBINATION THERAPY
It is the
combined use of drugs intended to achieve better action; in chemotherapy it is
used for the synergistic action (e.g. a sulphonamide used with trimethoprim to
produce additive action). Other examples are in the combination of β-lactamase
inhibition by clavulanic acid or sulbactum with amoxycillin or ampicillin for β-lacamase
producing H. influenza, Neisseria
gonorrhoeae, and other organisms.. Combination of bactericidal with a
bacteriostatic drug produces synergistic action. The combination therapy of
antimicrobials are also used in the treatment of mixed infection and initial
treatment of severe infections.
Related Topics
