Antidiuretic Hormone
| Home | | Pharmacology |Chapter: Essential pharmacology : Antidiuretics
It is a nonapeptide secreted by posterior pituitary (neurohypophysis) along with oxytocin.
ANTIDIURETIC HORMONE
It is a nonapeptide
secreted by posterior pituitary (neurohypophysis) along with oxytocin (see Ch. No. 23). It is synthesized in
the hypothalamic (supraoptic and paraventricular) nerve cell bodies as a large
precursor peptide along with its binding protein ‘neurophysin’, and is
transported down the axons to nerve endings in the median eminence and pars
nervosa. Osmoreceptors present in hypothalamus and volume receptors present in
left atrium, ventricles and pulmonary veins primarily regulate the rate of ADH
release governed by body hydration. Impulses from baroreceptors and higher
centres also impinge on the nuclei synthesizing ADH and affect its release. The
two main physiological stimuli for ADH release are rise in plasma osmolarity
and contraction of e.c.f. volume.
ADH secretion is
enhanced by angiotensin II, prostaglandins (PGs), histamine, neuropeptide Y and
ACh. It is inhibited by GABA and atrial natriuretic peptide (ANP). Opioids
have agentspecific action: while morphine stimulates ADH secretion, endogenous
opioid peptides are mostly inhibitory. These humoral mediators may play a role
in the modulation of ADH secretion.
The mammalian ADH is 8argininevasopressin (AVP); 8-lysinevasopressin (lypressin) is found
in swine and has been synthetically prepared. Other more potent and longer
acting peptide analogues of ADH having agonistic as well as antagonistic action
have been prepared.
ADH (Vasopressin) Receptors
These are G protein
coupled cell membrane receptors; two subtypes V1 and V2
have been identified, cloned and structurally characterized.
V1 Receptors
All vasopressin
receptors except those on renal CD cells and
some blood vessels are of the V1 type. These are further divided
into:
V1a present on vascular
and other smooth muscles, platelets,
liver, etc. and V1b localized to the anterior pituitary.
The V1
receptors function mainly through the phospholipase C–IP3/DAG
pathway—release Ca2+ from intracellular stores—causing vasoconstriction,
visceral smooth muscle contraction, glycogenolysis, platelet aggregation, ACTH
release, etc. These actions are augmented by enhanced influx of Ca2+ through
Ca2+ channels as well as by DAG mediated protein kinase C activation which
phosphorylates relevant proteins. V1 receptors, in addition,
activate phospholipase A2—release arachidonic acid resulting in generation of
PGs and other eicosanoids which contribute to many of the V1
mediated effects. Persistent V1 receptor stimulation activates
protooncogenes (possibly through IP 3/DAG pathway) resulting in growth
of vascular smooth muscle and other responsive cells.
V2 Receptors
These are located
primarily on the collecting duct (CD) cells in the
kidney—regulate their water permeability through cAMP production. Vasodilatory
V2 receptors are present in blood vessels.
The V2 receptors
are more sensitive (respond at lower concentrations) to ADH than are V1
receptors.
Selective peptide agonists and antagonists of the subtypes of
vasopressin receptors are:
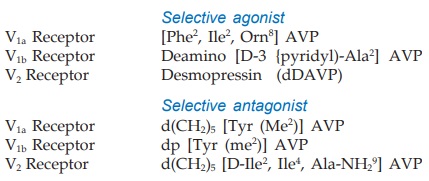
Some orally active
nonpeptide V1a and V2 receptor antagonists have been
produced and are under clinical trial.
Actions
Kidney
AVP acts on the
collecting duct (CD) cells to increase their
water permeability—water from the lumen diffuses to the interstitium by equilibrating
with the hyperosmolar renal medulla (see
Fig. IX.1). In man, maximal osmolarity of urine that can be attained is 4 times
higher than plasma. When ADH is absent, CD cells remain impermeable to water → dilute urine
(produced by the diluting segment) is passed as suCh. No. Graded effect occurs
at lower concentration of ADH: urine volume closely balances fluid intake.
Mechanism Of Action
The V2 subtype of ADH receptors are present on the basolateral side
of CD cell membrane. Activation of these receptors increases cAMP formation intracellularly
→ activation of cAMP
dependent protein kinase A → phosphorylation of relevant proteins which
promote exocytosis of ‘aquaporin2’
water channel containing vesicles (WCVs) through the apical membrane → more aqueous channels
get inserted into the apical membrane. The rate of endocytosis and degradation
of WCVs is concurrently reduced. The water permeability of CD cells is increased
in proportion to the population of aquaporin2 channels in the apical membrane
at any given time. Continued V2 receptor stimulation (during chronic
water deprivation) in addition upregulates aquaporin2 synthesis through cAMP
response element of the gene encoding aquaporin2.
Other aquaporins like
aquaporin1 (in PT) and aquaporin3,4 (on basolateral membrane of CD cells) also
participate in water transport at these sites.
To achieve maximum
concentration of urine, activation of V2 receptors increases urea
permeability of terminal part of CDs by stimulating a vasopressin regulated
urea transporter (VRUT or UT1)—which in turn augments medullary hypertonicity.
Recently, V2 receptor mediated actions of AVP on AscLH have been
demonstrated which further reinforce medullary hypertonicity by activating the
Na+K+2Cl¯ cotransporter in the shortterm and increasing its synthesis in the long-term.
The V 1
receptors also participate in the renal response to ADH. While V1a
receptor activation constricts vasa recta to diminish blood flow to inner
medulla which will help in maintaining high osmolarity in this region and thus
contribute to antidiuresis; other V1 actions augmenting PG
production from interstitial cells and directly diminishing responsiveness of CD
cells to V2 receptor stimulation tend to restrain V2
mediated water permeability. Since V2 action is produced at much
lower concentration of AVP, physiologically V1 renal actions may
serve to restrict V2 effect when blood levels of AVP are very high.
Lithium and
demeclocycline partially antagonize ADH action (probably by limiting cAMP
formation), reduce the urine concentrating ability of the kidney, produce polyuria
and polydipsia. They have been used in patients with inappropriate ADH
secretion. On the other hand NSAIDs (especially indomethacin) augment AVP
induced antidiuresis by inhibiting renal PG synthesis. Carbamazepine and
chlorpropamide also potentiate AVP.
Blood Vessels
AVP constricts blood
vessels through V1
receptors and can raise BP (hence the name vasopressin), but much higher concentration
is needed than for maximal antidiuresis. The cutaneous, mesenteric, skeletal
muscle, fat depot, thyroid, and coronary beds are particularly constricted.
Though vasoconstrictor action of AVP does not appear to be physiologically
important, some recent studies indicate that it may play a role in CHF,
haemorrhage, hypotensive states, etc. Prolonged exposure to AVP causes vascular
smooth muscle hypertrophy.
The V2
receptor mediated vasodilatation can be unmasked when AVP is administered in
the presence of a V1 antagonist. It can also be demonstrated by the
use of selective V2 agonist desmopressin, and appears to be EDRF
(NO) mediated.
Other Actions
Most visceral smooth muscles contract. Increased peristalsis in gut
(especially large bowel), evacuation and expulsion of gases may occur.
Uterus is contracted by AVP
acting on oxytocin receptors. In the
nonpregnant and early pregnancy uterus, AVP is equipotent to oxytocin. Only at
term sensitivity to oxytocin increases selectively.
CNS Exogenously
administered AVP does not penetrate blood-brain
barrier. However, it is now recognized as a peptide neurotransmitter in many
areas of brain and spinal cord: may be involved in regulation of temperature,
circulation, ACTH release, and in learning of tasks.
AVP induces platelet
aggregation and hepatic glycogenolysis. It releases coagulation factor VIII and
von Willebrand’s factor from vascular endothelium through V2
receptors.
Pharmacokinetics
AVP is inactive orally because it is destroyed by trypsin. It can be
administered by any parenteral route or by intranasal application. The peptide
chain of AVP is rapidly cleaved enzymatically in many organs, especially in
liver and kidney; plasma t½ is short~25 min. However, the action of aqueous
vasopressin lasts 3– 4 hours.
Aqueous vasopressin
(AVP) inj: POSTACTON 10 U inj; for i.v., i.m. or s.c. administration.
