Routes of Drug Administration
| Home | | Pharmacology |Chapter: Essential pharmacology : Introduction And Routes Of Administration
Most drugs can be administered by a variety of routes. The choice of appropriate route in a given situation depends both on drug as well as patient related factors. Mostly common sense considerations, feasibility and convenience dictate the route to be used.
ROUTES OF DRUG ADMINISTRATION
Most
drugs can be administered by a variety of routes. The choice of appropriate
route in a given situation depends both on drug as well as patient related
factors. Mostly common sense considerations, feasibility and convenience
dictate the route to be used.
Physical
and chemical properties of the drug (solid/liquid/gas; solubility, stability,
pH, irritancy).
Site
of desired action—localized and approachable or generalized and not
approachable.
Rate and extent of absorption of the drug from different routes.
Effect of digestive juices and first pass
metabolism on the drug.
Rapidity with which the response is desired
(routine treatment or emergency).
Accuracy of dosage required (i.v. and inhalational
can provide fine tuning).
Condition of the patient (unconscious, vomiting).
Routes can be broadly divided into those for
(a) Local action and
(b) Systemic action.
LOCAL ROUTES
These
routes can only be used for localized lesions at accessible sites and for drugs
whose systemic absorption from these sites is minimal or absent. Thus, high
concentrations are attained at the desired site without exposing the rest of
the body. Systemic side effects or toxicity are consequently absent or minimal.
For drugs (in suitable dosage forms) that are absorbed from these sites/routes,
the same can serve as systemic route of administration, e.g. glyceryl
trinitrate (GTN) applied on the skin as ointment or transdermal patch. The
local routes are:
Topical
This refers to external application of the drug to the
surface for localized action. It is often more convenient as well as
encouraging to the patient. Drugs can be efficiently delivered to the localized
lesions on skin, oropharyngeal/ nasal mucosa, eyes, ear canal, anal canal or
vagina in the form of lotion, ointment, cream, powder, rinse, paints, drops,
spray, lozengens, suppositories or pesseries. Nonabsorbable drugs given orally
for action on g.i. mucosa (sucralfate, vancomycin), inhalation of drugs for
action on bronchi (salbutamol, cromolyn sodium) and irrigating solutions/jellys
(povidone iodine, lidocaine) applied to urethra are other forms of topical
medication.
Deeper Tissues
Certain deep areas can be approached by using a
syringe and needle, but the drug should be such that systemic absorption is
slow, e.g. intraarticular injection (hydrocortisone acetate), infiltration
around a nerve or intrathecal injection (lidocaine), retrobulbar injection
(hydrocortisone acetate).
Arterial Supply
Close intraarterial injection is used for contrast
media in angiography; anticancer drugs can be infused in femoral or brachial
artery to localise the effect for limb malignancies.
SYSTEMIC ROUTES
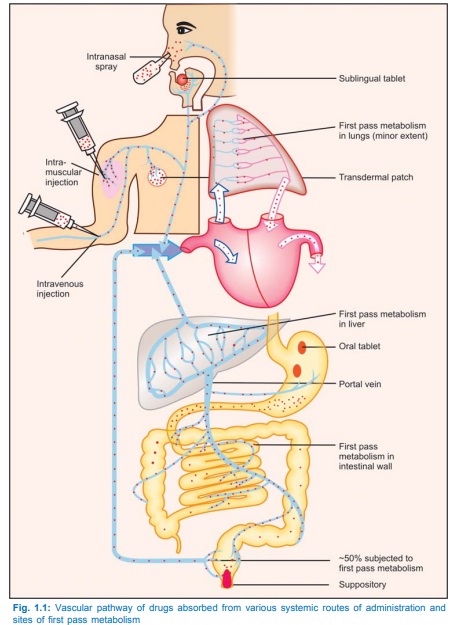
The drug administered
through systemic routes is intended to be absorbed into the blood stream and
distributed all over, including the site of action, through circulation (see Fig. 1.1).
1. Oral
Oral ingestion is the
oldest and commonest mode of drug administration. It is safer, more convenient,
does not need assistance, noninvasive, often painless, the medicament need not
be sterile and so is cheaper. Both solid dosage forms (powders, tablets,
capsules, spansules, dragees, moulded tablets, gastrointestinal therapeutic
systems—GITs) and liquid dosage forms (elixirs, syrups, emulsions, mixtures)
can be given orally.
Action of drugs is slower and thus not
suitable for emergencies.
Unpalatable drugs (chloramphenicol) are
difficult to administer; drug may be filled in capsules to circumvent this.
May
cause nausea and vomiting (emetine).
Cannot be used for
uncooperative/unconscious/vomiting patient.
Absorption of drugs may be variable and
erratic; certain drugs are not absorbed (streptomycin).
Others are destroyed by digestive juices (penicillin
G, insulin) or in liver (GTN, testosterone, lidocaine).
2. Sublingual (s.l.) or Buccal
The tablet or pellet containing the drug is
placed under the tongue or crushed in the mouth and spread over the buccal
mucosa. Only lipid soluble and nonirritating drugs can be so administered.
Absorption is relatively rapid—action can be produced in minutes. Though it is
somewhat inconvenient, one can spit the drug after the desired effect has been
obtained. The chief advantage is that liver is bypassed and drugs with high
first pass metabolism can be absorbed directly into systemic circulation. Drugs
given sublingually are—GTN, buprenorphine, desaminooxytocin.
3. Rectal
Certain
irritant and unpleasant drugs can be put into rectum as suppositories or
retention enema for systemic effect. This route can also be used when the
patient is having recurrent vomiting or is unconscious. However, it is rather inconvenient
and embarrassing; absorption is slower, irregular and often unpredictable,
though diazepam solution is rapidly and dependably absorbed from rectum in
children. Drug absorbed into external haemorrhoidal veins (about 50%) bypasses
liver, but not that absorbed into internal haemorrhoidal veins. Rectal
inflammation can result from irritant drugs. Diazepam, indomethacin,
paraldehyde, ergotamine and few other drugs are some times given rectally.
4. Cutaneous
Highly
lipid soluble drugs can be applied over the skin for slow and prolonged
absorption. The liver is also bypassed. The drug can be incorporated in an
ointment and applied over specified area of skin. Absorption of the drug can be
enhanced by rubbing the preparation, by using an oily base and by an occlusive
dressing.
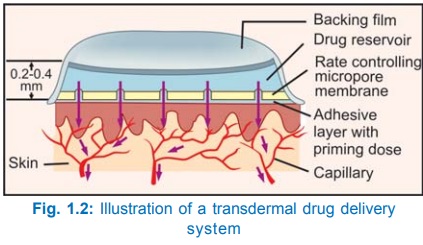
Transdermal Therapeutic Systems
These are devices in the form of adhesive patches of
various shapes and sizes (5–20 cm2) which deliver the contained drug at a
constant rate into systemic circulation via the stratum corneum (Fig. 1.2). The
drug (in solution or bound to a polymer) is held in a reservoir between an
occlusive backing film and a rate controlling micropore membrane, the under
surface of which is smeared with an adhesive impregnated with priming dose of
the drug. The adhesive layer is protected by another film that is to be peeled
off just before application. The drug is delivered at the skin surface by
diffusion for percutaneous absorption into circulation. The micropore membrane
is such that rate of drug delivery to skin surface is less than the slowest
rate of absorption from skin. This offsets any variation in the rate of
absorption according to the properties of different sites. As such, the drug is
delivered at a constant and predictable rate irrespective of site of
application: usually chest, abdomen, upper arm, lower back, buttock or mastoid
region are utilized.
Transdermal
patches of GTN, fentanyl, nicotine and estradiol are available in India, while
those of isosorbide dinitrate, hyoscine, and clonidine are available in other
countries. These have been designed to last for 1–7 days in case of different
drugs and are becoming increasingly popular, because they provide smooth plasma
concentrations of the drug without fluctuations; minimize interindividual
variations (drug is subjected to little first pass metabolism) and side
effects. They are also more convenient—many patients prefer transdermal patches
to oral tablets of the same drug; patient compliance is better. Local
irritation and erythema occurs in some, but is generally mild; can be minimized
by changing the site of application each time by rotation. Discontinuation has
been necessary in 2–7% cases.
5. Inhalation
Volatile liquids and
gases are given by inhalation for systemic action, e.g. general anaesthetics.
Absorption takes place from the vast surface of alveoli—action is very rapid.
When administration is discontinued the drug diffuses back and is rapidly eliminated
in expired air. Thus, controlled administration is possible with moment to
moment adjustment. Irritant vapours (ether) cause inflammation of respiratory
tract and increase secretion.
6. Nasal
The mucous membrane of
the nose can readily absorb many drugs; digestive juices and liver are
bypassed. However, only certain drugs like GnRH agonists and desmopressin
applied as a spray or nebulized solution have been used by this route. This
route is being tried for some other peptide drugs, like insulin.
7. Parenteral
(Par—beyond, enteral—intestinal)
This refers to
administration by injection which takes the drug directly into the tissue fluid
or blood without having to cross the intestinal mucosa. The limitations of oral
administration are circumvented.
Drug
action is faster and surer (valuable in emergencies). Gastric irritation and
vomiting are not provoked. Parenteral routes can be employed even in
unconscious, uncooperative or vomiting patient. There are no chances of
interference by food or digestive juices. Liver is bypassed.
Disadvantages
of parenteral routes are—the preparation has to be sterilized and is costlier,
the technique is invasive and painful, assistance of another person is mostly
needed (though self injection is possible, e.g. insulin by diabetics), there
are chances of local tissue injury and, in general, parenteral route is more
risky than oral. The important parenteral routes are:
(i)
Subcutaneous (s.c.)
The drug is deposited in the loose subcutaneous tissue which is
richly supplied by nerves (irritant drugs cannot be injected) but is less
vascular (absorption is slower than intramuscular). Only small volumes can be
injected s.c. Selfinjection is possible because deep penetration is not needed.
This route should be avoided in shock patients who are vasoconstricted—absorption
will be delayed. Repository (depot) preparations that are aqueous suspensions
can be injected for prolonged action. Some special forms of this route are:
a) Dermojet In this method needle is not used; a high velocity jet of drug solution is
projected from a microfine orifice using a gun like implement. The solution
passes through the superficial layers and gets deposited in the subcutaneous
tissue. It is essentially painless and suited for mass inoculations.
b) Pellet Implantation The drug in the form
of a solid pellet is
introduced with a trochar and cannula. This provides sustained release of the
drug over weeks and months, e.g. DOCA, testosterone.
c) Sialistic
(nonbiodegradable) and Biodegradable Implants Crystalline drug is
packed in tubes or capsules made of
suitable materials and implanted under the skin. Slow and uniform leaching of
the drug occurs over months providing constant blood levels. The
nonbiodegradable implant has to be removed later on but not the biodegradable
one. This has been tried for hormones and contraceptives (e.g. NORPLANT).
(ii)
Intramuscular (i.m.)
The
drug is injected in one of the large
skeletal muscles—deltoid, triceps, gluteus maximus, rectus femoris, etc. Muscle
is less richly supplied with sensory nerves (mild irritants can be injected)
and is more vascular (absorption of drugs in aqueous solution is faster). It is
less painful, but self injection is often impracticable because deep
penetration is needed. Depot preparations (oily solutions, aqueous suspensions)
can be injected by this route.
Intramuscular
injections should be avoided in anticoagulant treated patients, because it can
produce local haematoma.
(iii)
Intravenous (i.v.)
The drug is injected as a bolus (Greek: bolos–lump) or infused slowly over hours
in one of the superficial veins. The drug reaches directly into the blood
stream and effects are produced immediately (great value in emergency). The
intima of veins is insensitive and drug gets diluted with blood, therefore,
even highly irritant drugs can be injected i.v., but hazards are—
thrombophlebitis of the injected vein and necrosis of adjoining tissues if
extravasation occurs. These complications can be minimized by diluting the drug
or injecting it into a running i.v. line. Only aqueous solutions (not
suspensions) can be injected i.v. and there are no depot preparations for this
route. The dose of the drug required is smallest (bioavailability is 100%) and
even large volumes can be infused. One big advantage with this route is—in case
response is accurately measurable (e.g. BP) and the drug short acting (e.g.
sodium nitroprusside), titration of the dose with the response is possible.
However, this is the most risky route—vital organs like heart, brain, etc. get
exposed to high concentrations of the drug.
(iv)
Intradermal Injection
The
drug is injected into the skin raising
a bleb (e.g. BCG vaccine, sensitivity testing) or scarring/multiple puncture of the epidermis through a drop of the
drug is done. This route is employed for specific purposes only.
