Structures of the Heart
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: The Heart
The heart lies inside the thoracic cavity, resting on the diaphragm.
Structures
of the Heart
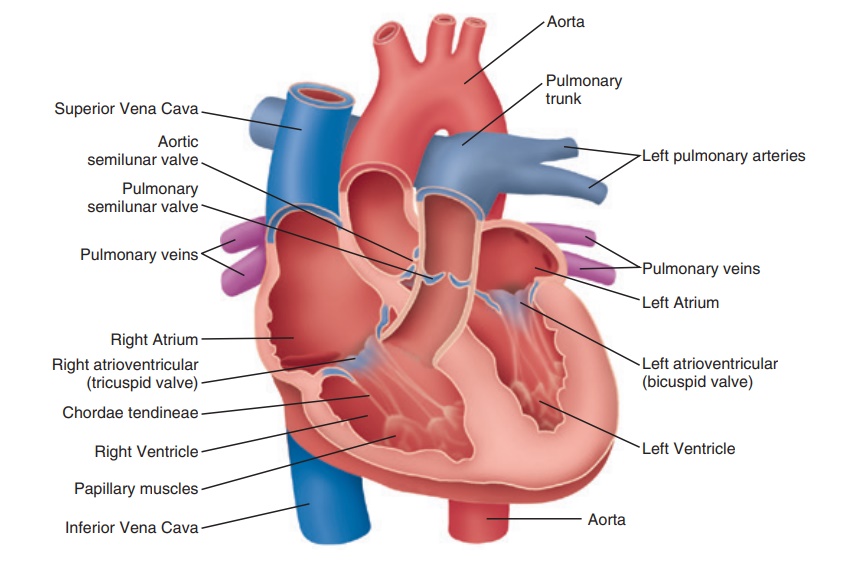
The heart lies inside the thoracic cavity, resting on the diaphragm (FIGURE 18-2). It is hollow and cone-shaped, varying in size. The heart is roughly the size of a man’s clenched fist. The heart is within the mediastinum, which is the medial cavity of the thorax, in between the lungs. Its posterior border is near the vertebral column, and its anterior border is near the sternum. It is not situated in the exact center of the thorax, and approximately two-thirds of the heart lies to the left of the midsternal line. It is partially obscured, laterally, by the lungs.
The average adult heart is about 14 cm (5 inches) long by 9
cm (3.5 inches) wide and weighs approx-imately 300 g. The base of the heart is actually the upper portion, where it is
attached to several large blood vessels. This wide portion of the heart lies
beneath the second rib. The distal end of the heart extends downward, to the
left, ending in a blunt point called the apex,
which is even with the fifth intercostal space. The apex points toward the left
hip. Just below the left nipple, between the fifth and sixth ribs, theapi-cal impulse can easily be felt. This
is caused by the apextouching the chest wall.
Coverings of the Heart
The heart is enclosed in the pericardium, a double-walled sac. Its superficial portion, the fibrouspericardium, is loose-fitting,
and consists of tough,dense connective tissue. It functions to protect the
heart, and anchor it to surrounding structures. The pericardium also prevents
the heart from becoming overfilled with blood. The serous pericardium lies deep to fibrous pericardium.
It is a thin and slippery membrane with two layers, and forms a closed sac
enclosing the heart. The parietal
layer of the serous pericardium lines the internal surfaces of
the fibrous pericardium.
At the heart’s superior margin, the parietal layer is
attached to the large arteries that exit the heart. The parietal layer then
turns inferiorly, continuing over the external surface of the heart as the visceral layer or epicardium, which is an important part of the heart wall. A
slit-like pericardial cavity lies
between the parietal and visceral layers. It contains a film of serous fluid.
The serous membranes are lubricated by this fluid. They move smoothly past each
other and allow the heart to work with very little friction.
Heart Layers
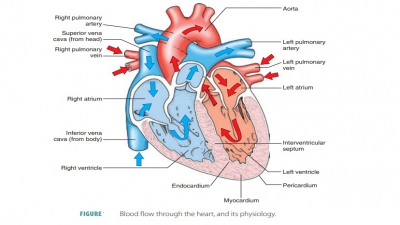
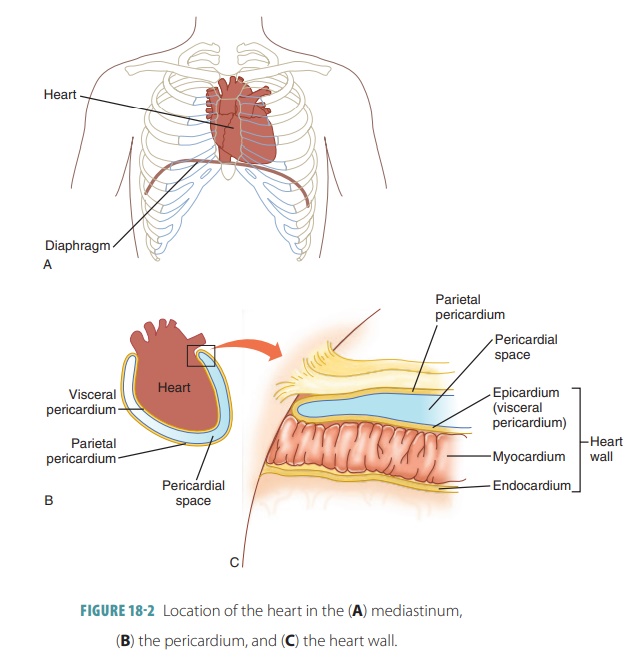
The three layers composing the wall of the heart are the
outer epicardium, middle myocardium, and inner endocardium (FIGURE 18-3). The epicardium protects the heart by reducing friction and is the visceral
por-tion of the pericardium on the
surface of the heart. It consists of connective tissue and some deep adipose
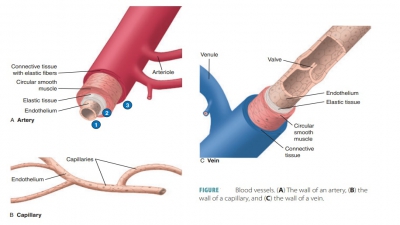
tissue. The middle layer, or myocardium, is made
mostly of cardiac muscle tissue that is organized in planes and richly supplied
by blood capillaries, lymph capillaries, and nerve fibers. It pumps blood out
of the chambers of the heart. The endocardium is made
up of squamous epithelium and connective tissue with many elastic and
collagenous fibers. The endocar-dium rests on the inner myocardial surface,
lining the chambers of the heart and covering the fibrous tissue that forms the
heart valves. It is continuous with endo-thelial linings of the heart’s blood vessels.
Heart Chambers and Great Vessels
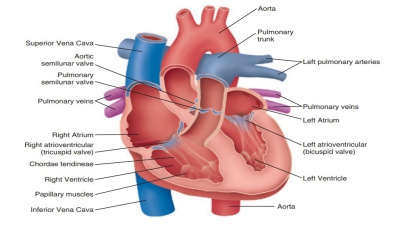
The four chambers of the heart are the rightatrium, right ventricle , left atrium, and left ventricle (Figure 18-3).
Each chamber receives blood in different ways. The upper chambers are called atria and receive blood returning to the heart. The lower
chambers are called ventricles and
receive blood from the atria, which they pump out into the arteries.
The left atrium and ventricle are separated from the right
atrium and ventricle by a solid wall-like struc-ture called septum. This keeps blood from one side of the heart from mixing
with blood from the other side, except in a developing fetus. There are smooth
sur-faces on the right atrium’s posterior wall and the inter-atrial septum.
However, prominent ridges of muscles known as pectinate muscles or musculi pectinati are found on the anterior atrial wall and inner
surface of the auricle.
The left atrium makes up most of thebase of the heart. Four pulmonary
veins enter the left atrium, carrying blood from the lungs. The
pulmonary veins are most easily seen in a posterior view of the heart. The
blood passes from the left atrium into the left ventricle through the left atrioventricular (A-V)valve ormitral valve, which prevents it from flow-ing
back into the left atrium from the ventricle. Like the tricuspid valve, the papillary muscles and chordae tendineae prevent the mitral valve’s cuspsfrom swinging
back into the left atrium when the ventricle contracts. The mitral valve closes
passively, directing blood through the large artery known as the aorta.
The left ventricle forms most of the apex and
inferoposterior area of the heart. The left ventricle is thicker because it
forces blood through the aorta to all
body parts, which have a much higher resistance to blood flow. The cavity of
the left ventricle is almost circular. The area where the septum separates the
right and left ventricles is marked on the heart’s surface by the anterior interventricular sulcus. This
groove cradles the anterior interventricular artery and con-tinues to become
the posterior interventricularsulcus.
This sulcus is visible on the posteroinferiorsurface of the heart.
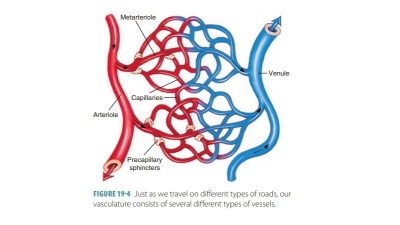
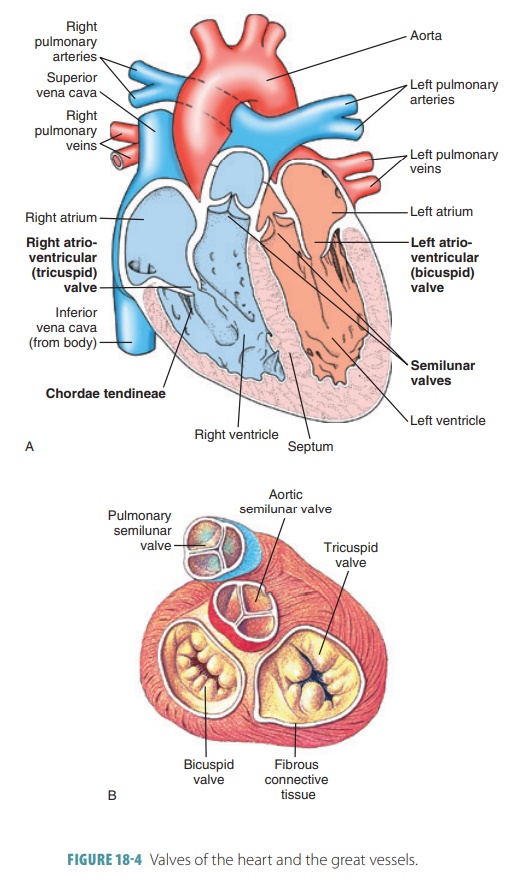
The right atrium receives blood from two large veins called
the superior vena cava and the inferiorvena cava and from a smaller vein
called thecoro-nary sinus, which
drains blood into the right atriumfrom the heart’s myocardium (FIGURE 18-4). The supe-rior vena
cava returns blood from areas of the body that are superior to the diaphragm,
whereas the infe-rior vena cava returns blood from areas of the body that are
inferior to the diaphragm. The right atrium sends blood to the right ventricle
through the tricus-pid valve. When each atrium is not filled with blood, its
outer portion deflates to resemble a wrinkled flap. This expandable atrial appendage is also called an auricle. The auricle slightly
increases blood volumein the atria.
The right ventricle forms most of the anterior sur-face of
the heart. Its muscular wall is about three times thinner than that of the left
ventricle, because it only pumps blood to the lungs, which have a low
resistance to blood flow. The inner surface of the right ventricle contains a
series of muscular ridges called trabeculaecarnae.
The cavity of the right ventricle is flatter thanthat of the left ventricle,
with a crescent shape and par-tially enclosing the left ventricle. As the right
ventricle contracts, its blood increases in pressure to passively close the
tricuspid valve. Therefore, this blood can only exit through the pulmonary trunk, which divides into the
left and right pulmonary arteries that supply the lungs. At the trunk’s base is
a pulmonary valve
that allows blood to leave the right ventricle while preventing
backflow into the ventricular chamber. The pulmonary valve contains three
cusps. Before the pul-monary valve, the superior end of the right ventricle
becomes tapered, forming a cone-shaped pouch called the conus arteriosus.
1. Explain the systemic and pulmonary circuits.
2. Where is the heart located?
3. Briefly explain the layers of the heart wall.
4. Why are the walls of the left ventricle thicker
than
those of the right ventricle?
5. Distinguish between the visceral pericardium
and the parietal pericardium.
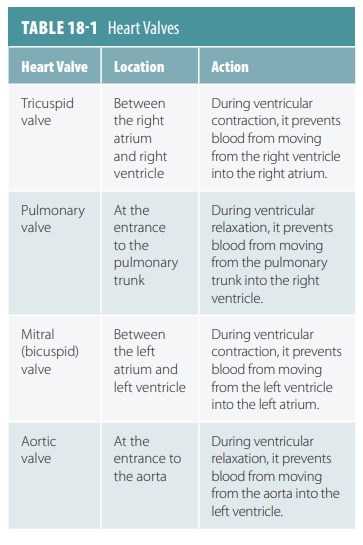
Heart Valves
The blood flow through the heart is in one direc-tion
because of the actions of the heart valves. The four heart valves open and
close because of pressure differences in each chamber. The four heart valves
are the two A-V valves and the two
semilunar valves.
A-V Valves
The tricuspid valve and bicuspid or mitral valve are known as A-V
valves because they lie between the atria and ventricles. They prevent
backflow or regurgitation
of blood from the ventricles to theatria while the ventricles
contract. The tricuspidvalve, also
known as the right A-V valve, has
threeflexible projections called cusps
and lies between the right atrium and ventricle. The cusps are actually flaps
of endothelium that are reinforced by cores of connective tissue. This valve
allows blood to move from the right atrium into the right ventricle while
preventing backflow. The cusps of the tricuspid valve are attached to strong
fibers called chordae
tend-ineae, which originate from smallpapillary musclesthat project inward from the ventricle walls.
These muscles contract as the ventricle contracts. When the tricuspid valve
closes, the papillary muscles pull on the chordae tendineae to prevent the
cusps from swinging back into the atrium.
The mitral valve
is located between the left atrium and left ventricle. It is also called the bicuspid valve because it has two cusps.
When the left atrium is filled with oxygenated blood, it pushes the mitral
valve open, sending the blood into the left ventricle. Figure 18-4 shows
various views of the heart valves.
Semilunar Valves
The pulmonary and aortic valves have half-moon shapes and
are therefore referred to as semilunar
valves. The pulmonary and aortic valves prevent backflow of blood
from the aorta and pulmonary trunk back into their associated ventricles. They
respond to pressure differ-ences, similar to the A-V valves. The semilunar
valves are forced open, causing their cusps to flatten against the artery walls
as blood moves past them. This occurs when the ventricles contract, increasing
intraventricu-lar pressure above the pressure in the aorta and pulmo-nary
trunk. When the ventricles are relaxed, the blood can then flow back toward the
heart, filling the cusps and closing the valves.
At the base of the aorta is the aortic valve, which has three cusps. This valve opens to allow blood to
leave the left ventricle during contraction and flow into the ascending aorta. Blood then flows
through the aortic arch and into the descending aorta . When the left
ventricle relaxes, the valve closes to prevent blood from backing up into the
ventricle. The pulmo-nary valve is
located in the right ventricle and opensto the pulmonary trunk to send
deoxygenated blood to the lungs. Near each cusp of the aortic valve are
sac-like structures called aortic
sinuses, which prevent the cusps from sticking to the aortic wall
as the valve opens. TABLE
18-1 summarizes the various heart valves.
Connective tissue arranged in “rings” surrounds the proximal
ends of the pulmonary trunk and aorta, providing firm attachments for heart
valves and mus-cle fibers. They prevent the outlets of the atria and
ven-tricles from dilating during contraction. These rings, as well as other
dense connective tissue masses, form the heart’s “skeleton.”
1. Identify the locations of the A-V and semilunar valves.
2. Explain the location and functions of the mitral valve.
3. Discuss the components that make up the “skeleton” of the
heart.
4. Explain the function of the chordae tendineae and the
papillary muscles.
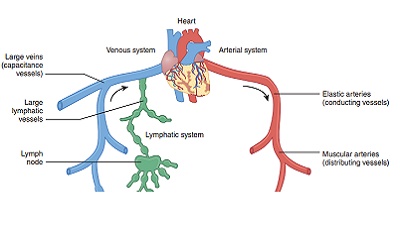
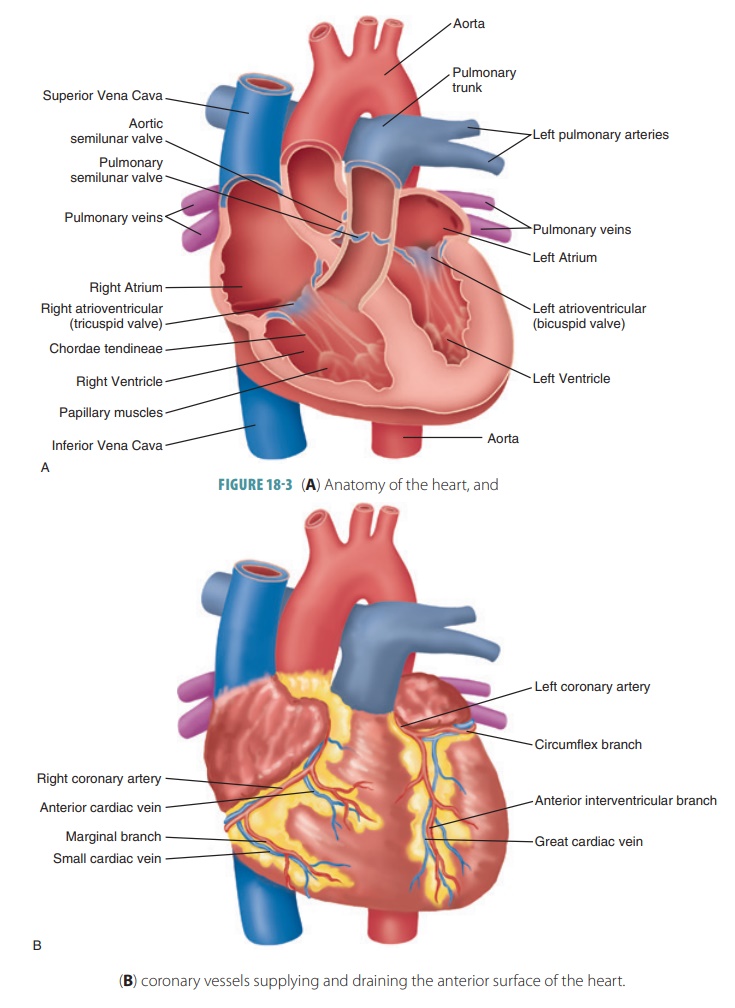
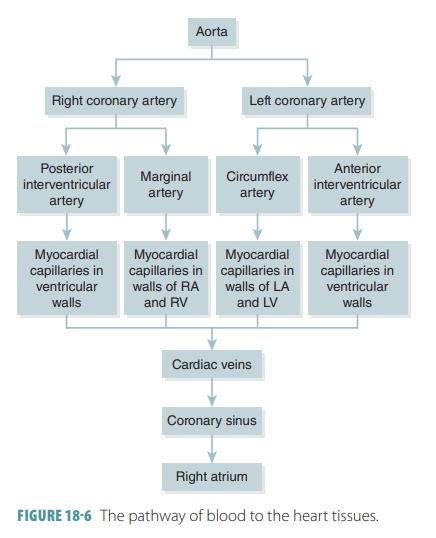
Heart Circulation
The heart is nourished via the coronary circulation. This is the shortest circulation in the
entire body and the functional blood supply of the heart. It is import-ant to
remember that blood flows through the heart in only one direction, controlled
by the four heart valves. The valves open and close as a result of differences
in pressure on their two sides.
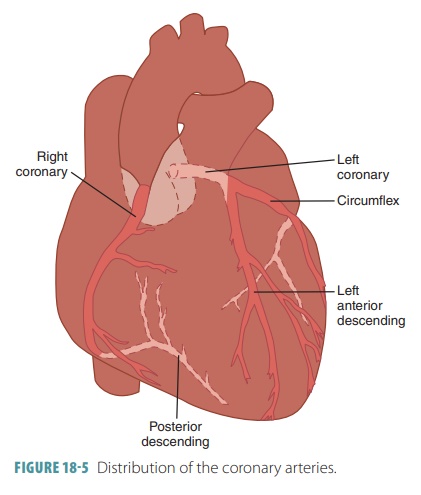
Coronary Arteries
The first two aortic branches are called the right and left coronary arteries. They supply blood to the heart
tissues, with openings lying just beyond the aortic valve. The coronary
arteries deliver blood when the heart is relaxed and have less function while
the ven-tricles are contracting because they are compressed by the myocardium.
Both of these coronary arteries enclose the heart in the coronary sulcus and provide the arterial
supply of the coronary circulation. The left coronary artery runs toward the left side of the
heart, whereas therightcoronary
artery runs toward the right side. The leftcoronary
artery is divided into the anterior
interven-tricular artery and thecircumflex
artery. The anteriorinterventricular artery is also known as the left anteriordescending artery. It
supplies blood to the anterior wallsof both ventricles and to the
interventricular septum. This artery follows the anterior interventricular sulcus. The circumflex artery supplies the posterior
walls of the left ventricle and the left atrium FIGURE( 18-5).
Coronary artery branches supply many capillaries in the
myocardium. These arteries have smaller branches with connections called anastomoses between vessels that provide
alternate blood path-ways. Known as collateral
circulation, these pathways may supply oxygen and nutrients to the
myocardium when blockage of a coronary artery occurs. The rightcoronary artery is divided into the right marginal artery and the posterior
interventricular artery. The right mar-ginal artery serves the myocardium
of the heart’s lateral right side. There also may be more than one marginal
artery. The posterior interventricular artery supplies the posterior
ventricular walls and runs to the heart apex. It merges oranastomosesnear the apex of theheart with the anterior interventricular artery.
Coronary Veins
The coronary
veins are basically located along the same paths as the coronary
arteries. They join to form the enlarged coronary sinus, emptying into the right atrium. On
the posterior aspect of the heart, the coronary sinus can easily be seen. It
empties into the great
cardiac vein, middle cardiac vein,and small
cardiac vein. Also, several anterior cardiac veins empty into the right
atrium’s anterior portion. The pos-terior
cardiac vein also empties into the great cardiacvein or coronary sinus. The
coronary sinus empties directly into the right atrium. FIGURE 18-6 illustrates the pathway
of blood to the heart tissues.
Heart Contraction
Some cardiac muscle cells are self-excitable, whereas each skeletal muscle fiber requires stimulation by a nerve ending to contract. Certain cardiac muscle cells are interconnected by intercalated discs, at which point interlocking membranes of nearby cells are linked by gap junctions and held together by desmosomes. The intercalated discs transfer the force of contractions from cell to cell and propagate action potentials.
There are three major differences between the ways in which
cardiac muscle and skeletal muscle contract. First, self -excitable cardiac
muscle cells can also initiate the depolarization of the rest of the heart,
spontaneously and with rhythm. This property is known as automaticity or autorhythmicity. Sec-ond, cardiac muscle has a property in which
either all heart fibers contract as a unit or not at all. This is coordinated
because all cardiac muscle cells are electrically linked together into one
contractile unit by gap junctions. As a result, the wave of depolar-ization
moves across the heart’s cells via ion passage along the gap junctions. All
this differs from skel-etal muscle, in which impulses do not spread from cell
to cell. Contraction of muscle fibers occurs from individual stimulation by
nerve fibers. Contraction is usually with just some of the motor units being activated.
Third, in cardiac muscle cells, the absolute refractory period lasts over 200
milliseconds (ms), which is almost as long as the contraction. This nor-mally
prevents tetanic contractions from occurring, which would stop the heart from
pumping. In skeletal muscle cells, contractions last only 15 to 100 ms and have
brief refractory periods of 1 to 2 ms. The abso-lute
refractory period is the period of no excitation,in which sodium ion
channels remain open or are inactivated. As a result of the long refractory
period, cardiac muscle cannot exhibit tetany.
Energy Requirements
Cardiac muscle needs much more oxygen for energy metabolism
than skeletal muscle and also has more mitochondria. The heart needs aerobic
respiration primarily. Therefore, without oxygen, cardiac muscle cannot operate
very well for very long. Skeletal muscle differs in that it can contract for a
long time via anaer-obic respiration and restore oxygen and fuel reserves via
excessive oxygen consumption after exercise.
Glucose, fatty acids, and other fuel molecules are used by
cardiac and skeletal muscle. However, because it is more adaptable, cardiac
muscle easily changes metabolic pathways so it can use whatever nutrients are
available. Such nutrients include lactic acid, which is generated by skeletal
muscle activity. Therefore, a lack of oxygen is much more dangerous to the
myo-cardium than any lack of nutrients.