Capillaries
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Vascular System
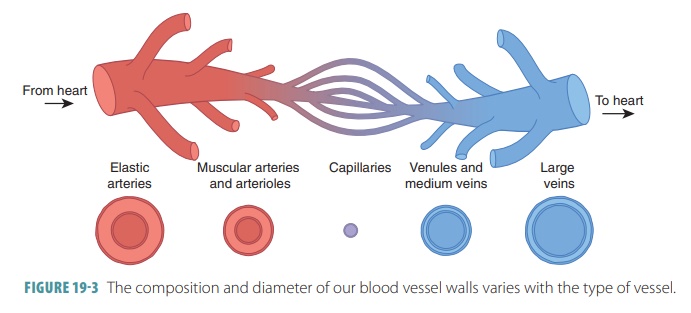
The smallest-diameter blood vessels are capillaries, which connect the smallest arterioles to the smallest venules.
Capillaries
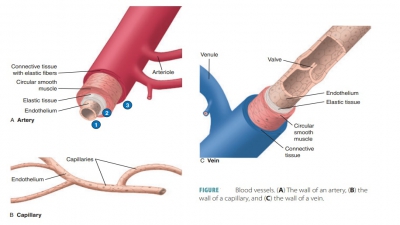
The smallest-diameter blood vessels are capillaries, which
connect the smallest arterioles to the smallest venules. The walls of
capillaries are also composed of endothelium and form the semipermeable layer
through which substances in blood are exchanged with substances in tissue
fluids surrounding cells of the body (FIGURE 19 -3). The capillaries are microscopic blood vessels with
extremely thin walls. Their walls contain a thin tunica intima and nothing
else. There-fore, this structure of the capillary wall differs from a vein or
an artery. Sometimes, a single endothelial cell makes up the entire
circumference of the wall of the capillary. There are three types of
capillaries, which include: continuous, fenestrated, and sinusoidal.
Continuous Capillaries
In continuous
capillaries, the
endothelium forms a complete lining. Most of the body is supplied with
continuous capillaries. Most capillaries average 1 mm in length with an average
lumen diameter of 8 to 10 μm, causing red blood cells to move through them one
at a time. Although most tissues have many capillaries tendons and ligaments
are examples of tissues that only have a small amount. These tissues get their
nutrients from the blood vessels of adjacent connec-tive tissues. In the eye,
the cornea and lens lack vessels, receiving nutrients from the aqueous humor.
Fenestrated Capillaries
In fenestrated
capillaries, window-like pores penetrate the endothelial lining, which
allow rapid exchange of solutes and water between the intersti-tial fluid and
plasma. Examples of these capillaries include the choroid plexus of the brain, and vessels in endocrine organs such
as the hypothalamus, pancreas, and pineal, pituitary, and thyroid glands.
Fenestrated capillaries are also located in absorptive areas of the intestinal
tract, and in the kidneys’ filtration sites. The amount of pores and levels of
permeability are differ-ent between various organs and between the actual
capillaries themselves.
Sinusoidal Capillaries
Sinusoidal
capillaries orsinusoidsare
similar tofenestrated capillaries but are more irregular in shape, with a
flattened appearance. Modified capillaries that are lined with phagocytes are
called sinusoids. These capillaries
have gaps between nearby endothelial cells. Their basement membrane is either
absent or very thin. They allow free exchange of solutes and water, including
plasma proteins, between interstitial fluid and blood. Through the sinusoidal
capillaries, blood moves slowly, which increases the time available for
exchange across the capillary walls. These capillaries are found in the bone
marrow, liver, spleen, and endo-crine organs such as the adrenal and pituitary
glands. In the liver, plasma proteins secreted by liver cells enter the
bloodstream. In the sinusoidal capillaries of the liver, bone marrow, and
spleen, phagocytic cells remove damaged red blood cells, cellular debris, and
pathogens from the blood.
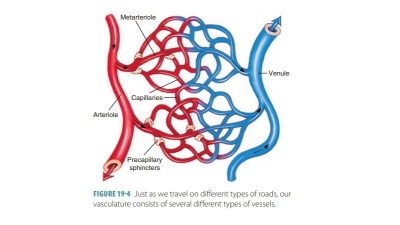
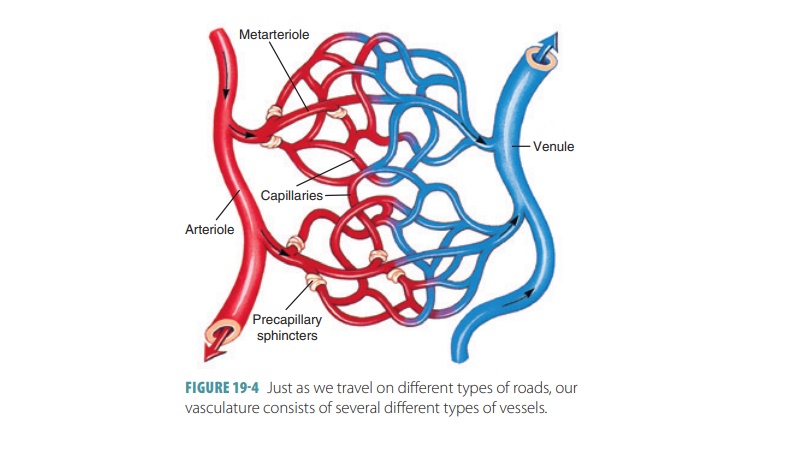
Capillary Beds
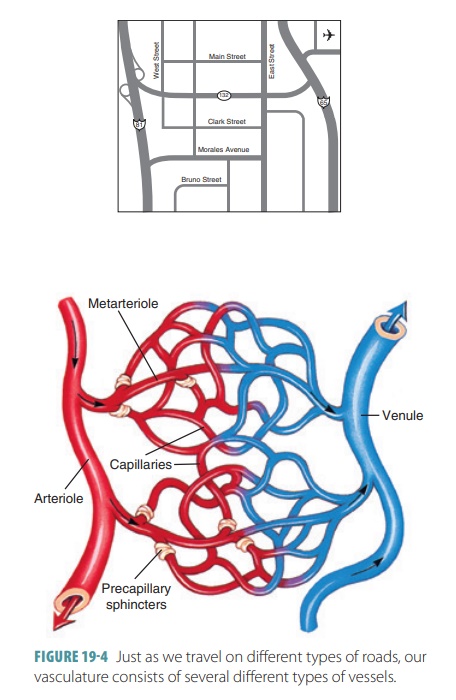
Capillaries form interwoven networks that are referred to as
capillary beds or capillary plexuses. The term microcirculation is used to describe
blood flowthrough the capillary beds, which lie between the arteri-oles and the
venules. Just one arteriole often connects to dozens of capillaries, which
empty into several venules. The two types of vessels in capillary beds, which
exist in most areas of the body, include true capillaries, which are the actual
exchange vessels, and vascular shunts,
also called metarterioles
or precapillary arterioles, which are
short vessels directly connecting arterioles and venules at opposite ends of
capillary beds.
A terminal
arteriole feeds the capillary bed via the metarteriole, which is
continuous with a thoroughfarechannel
between a capillary and a venule. This channelthen joins the postcapillary venule, which drains the
capillary bed. In each capillary bed, there are usually between 10 and 100
capillaries, varying per organ or type of body tissue. Most often, they branch
from the metarteriole, returning to the thoroughfare channel. However,
sometimes they emerge from the terminal arteriole, emptying directly into the
venule.
A precapillary
sphincter surrounds each true capillary’s root at the metarteriole.
This sphincter is a cuff of smooth muscle fibers that function as a valve, regulating
blood flow into the capillary. The blood that flows through a terminal
arteriole moves either through the true capillaries or through the vascu-lar
shunts. Open precapillary sphincters allow blood to flow through the true
capillaries for tissue cell exchanges. Closed precapillary sphincters cause
blood to flow through the vascular shunts, bypassing the tissue cells. More
than one artery can supply blood to a capillary bed. These multiple arteries
are known as collaterals,
and fuse before becoming arterioles. Thisfusion is an example of arterial anastomosis, such as in the
connections between the anterior and posterior interventricular arteries of the
heart.
The amount of blood that enters a capillary bed is regulated
by local chemical conditions as well as arte-riolar vasomotor nerve fibers.
Based on body or body region conditions, a capillary bed may be nearly full
with blood or bypassed almost totally. An example of differ-ing conditions
involves eating. After a meal the digestive process causes the blood to
circulate freely through the true capillaries of the gastrointestinal organs so
break-down products may be received for absorption by the body. As you approach
the time of your next meal and are getting hungry, the majority of these
capillary path-ways are closed. A different example involves vigorous exercise.
Blood is rechanneled from the digestive organs to the skeletal muscles, where
it is needed more. Vigorous exercise after a meal “confuses” the body’s
manage-ment of blood to the capillaries and may end up causing abdominal
problems such as cramping or indigestion.
Capillary walls have thin slits where endothelial cells
overlap. These slits have various sizes, affect-ing permeability. Capillaries
of muscles have smaller openings than those of the glands, kidneys, and small
intestine. Tissues with higher metabolic rates, such as muscles, have many more
capillaries than those with slower metabolic rates, such as cartilage.
Some capillaries pass directly from arterioles to venules,
whereas others have highly branched net-works (FIGURE 19-4). The precapillary sphincters con-trol blood distribution
through capillaries. Based on the demands of cells, these sphincters constrict
or relax so blood can follow specific pathways to meet tissue cellular
requirements. Gases, metabolic byproducts, and nutrients are exchanged between
capillaries and the tissue fluid surrounding body cells. Capillary walls allow
diffusion of blood with high levels of oxygen and nutrients and also allow
high levels of carbon dioxide and other wastes to move from the tissues into
the capillaries. Diffusion occurs also between the blood and interstitial fluid
in capillaries.
Plasma proteins usually cannot move through the capillary
walls because of their large size, so they remain in the blood. Blood pressure
generated when capillary walls contract provides force for filtration via
hydrostatic pressure. Blood pressure is strongest when blood leaves the heart
and weaker as the distance from the heart increases because of friction known
as peripheral resistance between
the blood and the vessel walls. Therefore, blood pressure is highest in the
arteries, less so in the arterioles, and lowest in the cap-illaries. Filtration
occurs mostly at the arteriolar ends of capillaries because the pressure is
higher than at the venular ends. Plasma proteins trapped in capillaries create
an osmotic pressure that pulls water into the capillaries, known as colloid osmotic pressure.
Capillary blood pressure favors filtration, whereas plasma
colloid osmotic pressure favors reabsorption. At the venular ends of
capillaries, blood pressure is decreased because of resistance so reabsorption
can occur. The capillaries of the body provide direct access to most cells and
are perfectly located and formed to easily exchange gases, hormones, nutrients,
and other components between the interstitial fluid and blood.
Angiogenesis is the formation of new bloodvessels. It is directed by vascular endothelialgrowth factor (VEGF).Angiogenesis occurs in anembryo as the tissues and organs develop. It can also occur at other times in body tissues as a response to factors released by cells that are oxygen-starved or hypoxic. Angiogenesis is most clinically important inthe heart, where it occurs because of chronic constric-tion or occlusion of blood vessels.
1. Identify three types of capillaries.
2. What is the role of the precapillary sphincters?