Blood Circulation
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Vascular System
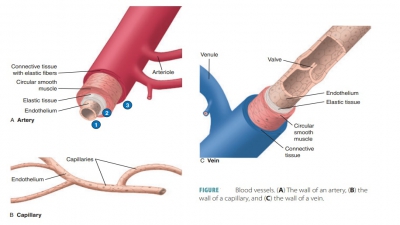
The blood must continue to circulate to sustain life. The heart acts as the circulation pump, and the arteries are pressurized reservoirs and channels.
Blood
Circulation
The blood must continue to circulate to sustain life. The
heart acts as the circulation pump, and the arteries are pressurized reservoirs
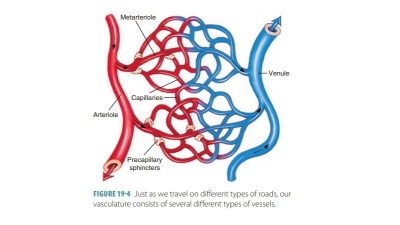
and channels. The arterioles control distribution of blood via resistance, the
capillaries provide sites for exchange, and the venules and veins collect
blood, acting as reservoirs and conducts. It is essential to define three
related terms: blood flow, blood
pressure, and resistance:
■■ Blood flow: The amount orvolumeof bloodthat flows through blood vessels, organs, or
thesystemic circulation, in milliliters per minute (mL/min). Throughout the
body, blood flow is equivalent to cardiac output. When resting, this is
relatively constant, yet in certain body organs, blood flow may be different
from others because of individual requirements. For example, blood flow to the
skin increases when environmental temperature rises. Brain blood flow
autoregulation is abolished when abnormally high carbon dioxide levels
persist.
■■ Blood pressure: It is
defined as the force thatblood exerts against the inner walls of blood vessels.
It most commonly refers to pressure in arteries supplied by the aortic
branches, even though it actually occurs throughout the vascu-lar system. Blood
flow is generated by the heart’s pumping action, and blood pressure results
from resistance opposing blood flow. Blood pressure is expressed in millimeters
of mercury (mm Hg). A blood pressure of
120 mm Hg is the same as a column of mercury that is 120 mm in height.
■■ Resistance: The friction
between blood and bloodvessel walls. Blood pressure must overcome this force
for the blood to continue flowing. Factors that alter peripheral resistance
therefore change blood pressure. Viscosity is
defined as the ease with which a fluid’s molecules flow past one another. The
higher the viscosity, the greater the resistance to flow. Blood viscosity is
increased by blood cells and plasma proteins. The greater the resistance, the
more force needed to move the blood. Blood pressure rises as blood viscosity
increases, and vice versa. Conditions such as exces-sive numbers of red blood
cells, which is known as polycythemia, can
cause both blood viscosity and resistance to increase. Some anemias, which
cause low red blood cell counts, reduce viscosity and peripheral resistance.
Total blood vessel length and resistance are inter-related.
There is more resistance over a longer vessel length in comparison with a
shorter vessel length. As an infant grows as a child and then an adult, blood vessels
lengthen. Therefore, the individual’s blood pressure and peripheral resistance
increase with growth. In healthy people blood viscosity and vessel length are
basically constant because they are rela-tively unchanging once adulthood is
reached. Blood vessel diameter changes often, however, and this does change
peripheral resistance. Fluid near a channel or tube wall slows down because of
friction. How-ever, in the center of the channel or tube, fluid flows quicker
since it experiences less friction. The smaller is a channel or tube, the
greater is the friction. This is because more of the fluid contacts the walls,
slowing its movement.
When the blood experiences a quick change in ves-sel
diameter, or the tube wall has protruding or rough areas, often due to
atherosclerotic plaques, the smooth laminar blood flow becomes turbulent flow. This is an irregular
fluid motion. Blood from different lamina, or layers of the tube’s cross
section, mix. The turbu-lence that is produced greatly increases resistance. Other
factors may increase peripheral resistance, such as when sympathetic
stimulation or epinephrine levels in the blood are increased.
Relationship Between Flow, Pressure, and Resistance
Blood pressure is calculated by multiplying cardiac output
by peripheral resistance. Normal arterial pres-sure is maintained by regulating
these two factors. Ideally, the volume of blood discharged from the heart
should be equal to the volume entering the atria and ventricles. Fiber length
and force of contraction are interrelated, because of the stretching of the
cardiac muscle cell just before contraction. Known as the Frank-Starling law of the heart, it is important duringexercise
when greater amounts of blood return to the heart from the veins.
Peripheral resistance also controls blood pres-sure. Changes
in the diameters of arterioles regulate peripheral resistance. The vasomotor center of the medulla oblongata controls
peripheral resistance.When arterial blood pressure increases suddenly,
baroreceptors in the aorta and carotid arteries alert the vasomotor center,
which vasodilates the vessels to decrease peripheral resistance. Carbon
dioxide, oxygen, and hydrogen ions also influence peripheral resistance by
affecting precapillary sphincters and smooth arteriole wall muscle.