Microscopic Anatomy (Bone Cells)
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Support and Movement: Bone Tissues and the Skeletal System
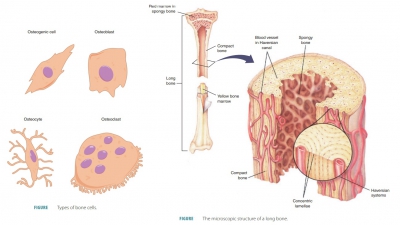
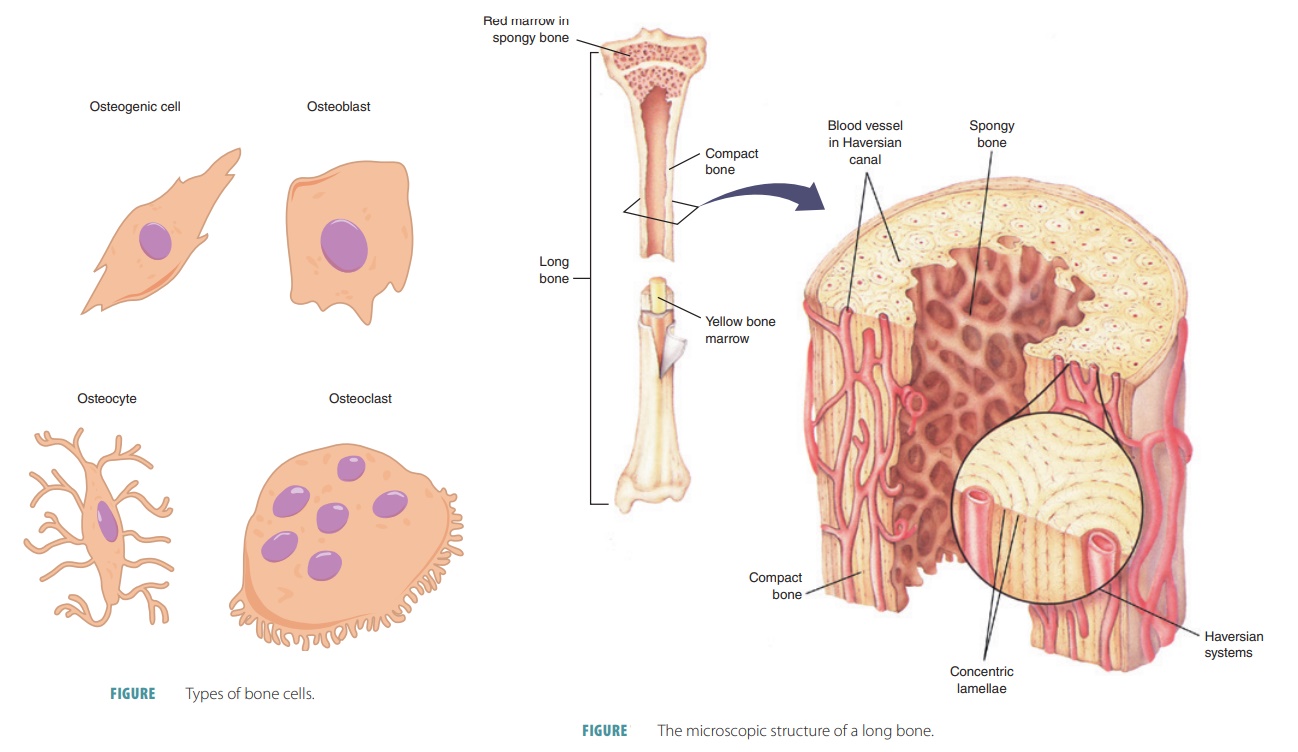
The five major types of bone cells are osteogenic cells, osteoblasts, osteocytes, bone lining cells , and osteoclasts.
Microscopic
Anatomy (Bone Cells)
The five major types of bone
cells are osteogenic cells, osteoblasts, osteocytes, bone lining
cells , and osteoclasts. All except osteoblasts originate from
mesenchymal cells. Each is basically a
specialized form of the certain cell type that becomes mature or functions in a
certain process involved in bone growth. Like various connective tissue cells,
bone cells are also surrounded by their own self-made extracellular matrix. The
five types are explained in detail as:
■■ Osteogenic cells:
Also known as osteoprogenitor cells, these mitotically active stem cells are
found in the periosteum and endosteum. They are squamous or flattened cells
when bones are growing. Stimulation of these cells causes them to often
differentiate into osteoblasts or bone lin-ing cells; others may remain as
osteogenic cells (FIGURE 7-4).
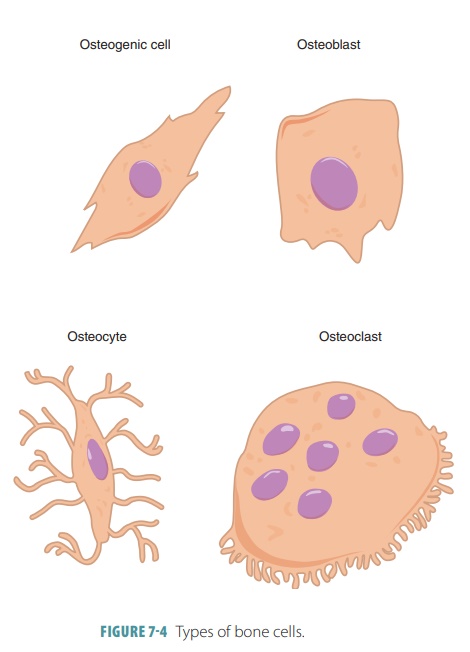
■■ Osteoblasts: These
cells produce bone matrix and are related to osteoprogenitor cells,
osteocytes,fibroblasts, and chondroblasts. They are mitotic and become active
with connective tissue layers, depositing bony matrix around them. Spongy bone
tissue forms in all directions within the layers of connective tissues. They
secrete an unmineralized bone matrix that includes colla-gen (which makes up
the majority of bone pro-tein) and calcium-binding proteins that form the
original unmineralized bone ( osteoid). They also aid in matrix calcification.
Osteoblasts are cube-shaped when they are depositing matrix, but appear similar
to flattened osteogenic cells when inactive. They may also differentiate into
bone lining cells. Osteoblasts become osteocytes when they are totally
surrounded by the matrix they are secreting.
■■ Osteocytes: These
are mature osteoblasts that have become embedded in the bone matrix. They
occupy small cavities (lacunae) in the bone and have protoplasmic projections
con-nected with the same structure of other osteo-cytes. The osteocytes conform
to the shapes of the lacunae. These connections form a system of tiny canals
within the bone matrix and act to maintain it as needed. When osteocytes die,
the matrix surrounding them is resorbed. They also react to strain or stress
and respond to stimuli such as bone deformation, bone loading, and
weightlessness. The osteocytes alert the osteo-blasts and osteoclasts to build
up or degrade the bone matrix as needed. This preserves calcium homeostasis.
■■ Bone lining cells: These are flat cells on bone sur-faces where bone remodeling does not occur and are believed to also help maintain the bone matrix. On external bone surfaces, they are called periosteal cells , and when they line internal sur-faces, they are called endosteal cells.
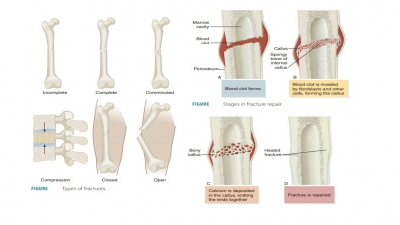
■■ Osteoclasts: These are large,
multinucleated bone cells found at
sites of bone resorption, which is called osteolysis.
They form from the hema-topoietic stem cells that also differentiate into
macrophages. During fractures and bone heal-ing and certain disease processes,
osteoclasts use enzymes to excavate passages (resorption bays) through
the surrounding tissue, breaking down
the calcified extracellular matrix. At this point, they have an irregular border that con-tacts bone
directly. This border has deep plasma membrane infoldings that greatly increase
the surface area for bone degradation via enzyme activity. The infoldings close
off the surface area from the matrix surrounding it. Osteoclasts are also known
as osteophages. They secrete an acid that dissolves the matrix. They resorb bone
matrix throughout life, replacing it with osteoblasts. These opposing
processes (resorp-tion and deposition) are regulated by hormones that control blood
calcium.
Compact Bone
Bone cells called osteocytes
occupy small chambers (lacunae) that create concentric circles around cen-tral
canals in bones (FIGURE 7-5). Cellular processes passing through canaliculi allow osteocytes to com-municate with other cells. Bone tissue is
mostly made up of collagen and inorganic salts such as calcium phosphate.
Calcium phosphate interacts with calcium hydroxide to form crystals of hydroxyapatite. These crystals
incorporate various calcium salts as well as ions such as fluoride, magnesium,
and sodium. Com-pact bones have a central canal that helps to make up
cylinder-shaped osteons or Haversian
systems. The osteons are parallel to the bone’s long axis, aid in weight bearing, and are
the structural units of compact bone. Each osteon consists of a group of
hol-low tubes of bone matrix that appear like the rings in a tree trunk. Each lamella (matrix
tube) lends its name to the other description of compact bone, which is lamellar bone.
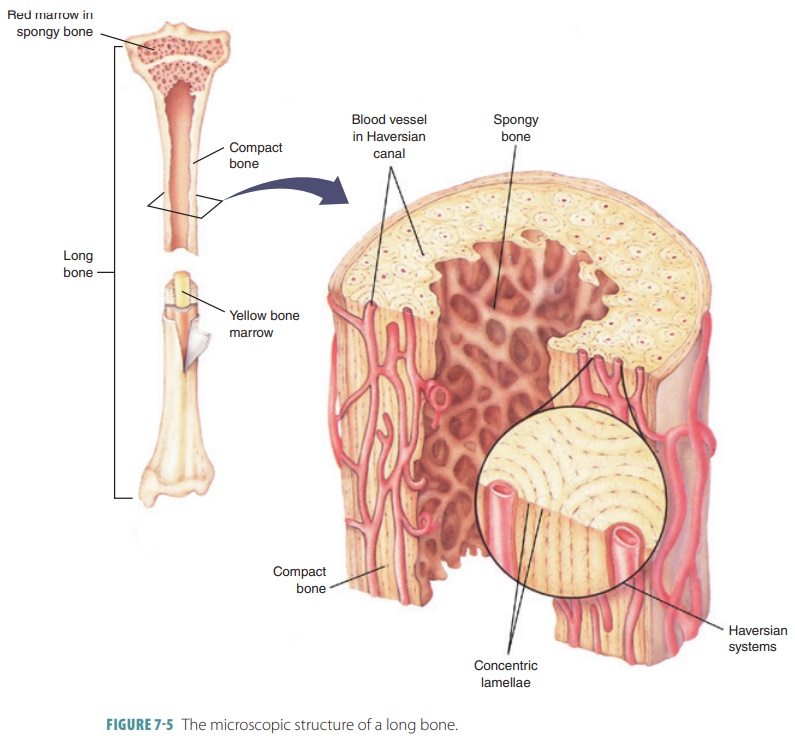
The collagen fibers of each
lamella run in one direction, whereas those in nearby lamellae run in
different directions. This alteration of collagen fiber placement strengthens
compact bone and resists twisting motions. Between collagen fibrils, bone salt
crystals also are aligned with directional alterations. Each central canal
contains nerve fibers, blood vessels and the surrounding connective tissue. The
central canals are connected by perforating Volkmann’s canals, which contain larger nerves and blood ves-sels. The
Volkmann’s canals lie at right angles to the long axis of the bone. They are
not surrounded by con-centric lamellae, but are lined with endosteum. At the
junctions of the lamellae are spider-shaped osteocytes occupying the lacunae. Thin, hair-like canaliculi con-nect lacunae to each
other and to the central canal. During bone formation, the osteoblasts that
secrete bone matrix surround blood vessels and stay in con-tact with each
other, as well as nearby osteocytes, via projections that extend outward. Each
of these exten-sions contains gap junctions. As the matrix hardens, a system of
canaliculi is formed, containing tissue fluid and the osteocytes’ extensions. A
mature osteon is then bound together, and both nutrients and wastes can move
from one osteocyte to the next. The bone matrix, therefore, allows bone cells
to receive nour-ishment while it still remains hard and impermeable. However,
some lamellae in compact bone are not part of complete osteons. Between osteons
are incomplete interstitial lamellae that either fill gaps or are leftover structures of
previous osteons that experienced bone remodeling.
Deep to the periosteum, just superficial to the endosteum, are circumferential lamellae, which
extend completely around the diaphysis, help-ing the long bone to resist
twisting.
Spongy Bone
Spongy bone is similarly composed
as compact bone, but its cells do not aggregate around the central canals. The
cells in spongy bone lie inside the trabeculae
(supporting structures of dense tissue) and take their nutrients from diffused
substances that enter the can-aliculi. The trabeculae are only a few cells
thick. They have irregular lamellae and osteocytes, interconnected by
canaliculi, and no osteons are present. Nutrients reach spongy bone osteocytes
via diffusion through the canaliculi from capillaries in the endosteum that
surround the trabeculae.
1. Compare
the structure of compact bone with spongy bone.
2. List
various types of bone cells and their functions.
3. Identify
osteons and lamellae.
Related Topics