Control of Breathing
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Respiratory System
Respiratory control has both involuntary and voluntary components. The involuntary centers of the brain regulate the respiratory muscles. They control respiratory minute volume by adjusting the depth and frequency of pulmonary ventilation.
Control
of Breathing
Respiratory control has both involuntary and voluntary
components. The involuntary centers of the brain regulate the respiratory
muscles. They control respiratory minute volume by adjusting the depth and
frequency of pulmonary ventilation. This occurs in response to sensory
information that arrives from the lungs, various portions of the respiratory
tract, and a variety of other sites.
The respiratory
areas of the brain control inspi-ration as well as exhalation.
The voluntary control of respiration reflects activity in the cerebral cortex
that affects either the output of the respiratory center in the medulla
oblongata and pons or the output of motor neurons in the spinal cord that
control respira-tory muscles. The most important parts comprise the medullary respiratory center,
which consists of the dorsal
and ventral respiratory groups and the respira-tory group of the pons (FIGURE 21-17).
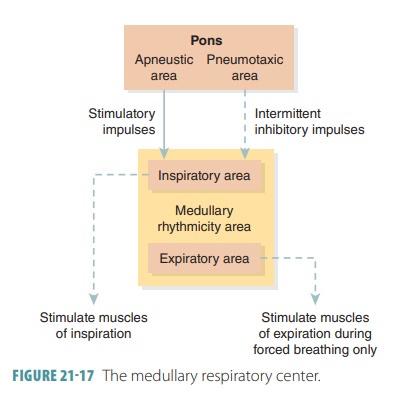
The dorsal respiratory group is located near the root of
cranial nerve IX. It is important in stimulating the muscles of inspiration but
is still not fully under-stood. Increased impulses result in more forceful
muscle contractions and deeper breathing. Decreased impulses result in passive
expiration. It is known that the dorsal respiratory group integrates input from
chemoreceptors and peripheral stretch receptors. It communicates this
information to the ventral respiratory group.
The ventral respiratory group controls other respiratory muscles, mostly the intercostals and abdominals, to increase the force of expiration and sometimes to increase inspiratory efforts. It is believed to be a center of integration and generation of rhythm. It is a network of neurons extending from the spinal cord, through the ventral brain stem, to the pons–medulla junction. Some neurons fire during inspiration, whereas others fire during expiration. The inspiratory neurons send impulses along the phrenic and intercostal nerves, exciting the diaphragm and external intercostal muscles, respectively. Therefore, damage to the phrenic nerves can increase respira-tory rate. The expiratory neurons cause the output to stop and passive expiration to occur, as the inspiratory muscles relax and the lungs then recoil.
This inspiratory and expiratory cycling is contin-uous,
producing the normal respiratory rate of 12 to 15 breaths per minute.
Inspiratory phases last about two seconds, whereas expiratory phases last about
three seconds. Eupnea is the term
describing this nor-mal respiratory rate and rhythm. In severe hypoxia, the
ventral respiratory group causes the individual to gasp for air. This may be a
final effort to restore oxygen to the brain. When certain clustered neurons are
completely suppressed, respiration stops. Causes of this include overdoses of
alcohol or drugs such as morphine.
The basic rhythm of breathing may also be con-trolled by the
pontine respiratory group in the pons. This consists of several centers
influencing and modi-fying medullary neuron activities. The pontine group is
believed to make the transitions between inspiration and expiration and the
reverse, smoother processes. Lesions to the superior region of the pontine
respi-ratory group cause prolonged inspirations to occur, which is called apneustic breathing.
However, the rhythmic quality of breathing is not fully
understood. The most accepted theory is that normal respiratory rhythm is based
on reciprocal inhi-bition of interconnected networks of neurons in the medulla.
Instead of one set of “pacemaker neurons,” two sets of neurons inhibit each
other. Their activity occurs in cycles, and this generates respiratory rhythm.
Factors of Respiratory Rate and Depth
The depth of inspiration during breathing is based on the
level of activity of the respiratory center and its stimulation of motor
neurons that serve the respira-tory muscles. With more stimulation, increased
num-bers of motor units are excited. Therefore, respiratory muscles contract
with greater force. Respiratory rate is established by the length of time the
inspiratory center is active or how fast it is turned off. Deep breathing is
referred to as diaphragmatic breathing, while shallow breathing is known as
costal breathing.
Certain chemicals also affect respiratory rate and depth.
Important substances include CO2, hydrogen, and oxygen ions in the
arterial blood. Other factors include emotional states, lung stretching capability,
and levels of physical activity. Chemosensitive areas known as central chemoreceptors, located in the medulla oblongata,
sense CO2 and hydrogen ion changes in the cerebrospinal fluid. When
these levels change, respira-tory rate and TV are signaled to increase. More CO2
is exhaled, and both blood and cerebrospinal fluid levels of these chemicals
fall, decreasing breathing rate.
CO2 is the most important chemical regulator of
respiration. Arterial partial pressure of CO2 is usually 40 mm Hg,
maintained within 3 mm Hg of this level, mostly by how rising CO2
levels affect the central che-moreceptors. Hypercapnia is a condition in which CO2 accumulates in the
brain. The accumulating CO2 is hydrated and H2CO3
is formed. When the acid is dissociated, hydrogen ions are freed and pH drops.
This also happens when CO2 enters red blood cells.
Increased hydrogen ions excite the central chemore-ceptors,
which extensively synapse with the respiratory regulatory centers. Breathing
depth and rate, therefore, increase. Because alveolar ventilation is enhanced,
CO2 is quickly flushed out of the blood and pH rises. Alveolar
ventilation is doubled with an elevation of only 5 mm Hg in arterial partial
pressure of CO2. This is true even when there is no change in
arterial oxygen levels or pH. The response to elevated partial pressure of CO2
is even more extensive when partial pressure of oxygen and pH are lower
than normal. Increased ventilation is usually self-limited. It stops when there
is restoration of homeostatic blood partial pressure of CO2.
The rising levels of hydrogen ions within the brain increase
the activity of the central chemoreceptors, even though rising blood CO2
is the first stimulus. Although hydrogen does not easily diffuse across the
blood–brain barrier, CO2 accomplishes this with no problem.
Therefore, control of breathing while resting mostly is based on regulation of
hydrogen ion concen-tration in the brain.
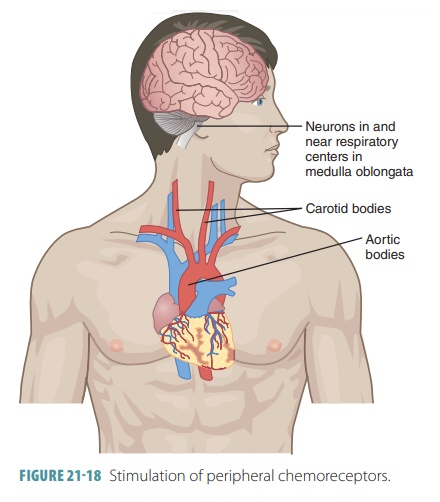
However, peripheral
chemoreceptors in the carotid and aortic bodies also help and are able to
sense changes in blood oxygen levels (FIGURE 21-18). Then, they increase the breathing rate, but this action
requires extremely low levels of blood oxygen to occur.
The depth of breathing is regulated by the inflation reflex, which occurs when stretched lung tissues
stimu-late stretch receptors in the visceral pleura, bronchioles, and alveoli.
The duration of inspiratory movements is shortened, preventing overinflation
of the lungs during forceful breathing. Emotional upset such as that caused by
fear and pain usually increase breathing rate. If breathing stops, even for a
short time, blood levels of CO2 and hydrogen ions rise and oxygen
levels fall. Chemoreceptors are stimulated and the urge to inhale increases,
overcoming the lack of oxygen. The deflation
reflex usually
only functions during forced exhalation and inhibits the expiratory centers while
stimulating the inspiratory centers when the lungs are deflating.
How Partial Pressure of Oxygen Influences Breathing
The peripheral chemoreceptors contain cells that are
sensitive to arterial levels of oxygen. These chemo-receptors lie in the aortic bodies of the aortic arch and the carotid bodies at the bifurcation of the com-mon
carotid arteries. Those in the carotid bodies are the main oxygen sensors.
Normally, reducing par-tial pressure of oxygen only affects ventilation
mini-mally. This primarily involves enhanced sensitivity of peripheral
receptors to increased partial pressure of CO2. For oxygen levels to
become a strong stimulus for increased ventilation, arterial partial pressure
of oxygen must drop greatly, to at least 60 mm Hg.
How Arterial pH Influences Breathing
Even during normal levels of oxygen and CO2,
changes to arterial pH can modify the rate and rhythm of breathing. Increased
ventilation occurring because of reduced arterial pH is controlled via the
peripheral chemoreceptors. This is in part because hydrogen ions do not cross
the blood–brain barrier. Changes in par-tial pressure of CO2 and
hydrogen ion concentration are related, yet different.
Reduced blood pH may be related to retention of CO2.
However, it may also occur because of meta-bolic reasons. These include lactic
acid accumulation because of exercise or fatty acid metabolite or ketone body accumulation because of
uncontrolled diabetes mellitus. No
matter what the reason, as arterial pH declines, the respiratory system will
attempt to com-pensate and raise the pH. This occurs by the increase of
respiratory rate and depth in an attempt to elimi-nate CO2 and H2CO3
from the blood.
How Higher Brain Centers Influence Breathing
Respiratory rate and depth are modified when pain or strong
emotions send signals to the respiratory centers. This occurs via the limbic
system, including the hypothalamus. Changes in body temperature also affect
respiration, with hotter temperatures increasing it and colder temperatures
decreasing it.
Conscious control of breathing can also occur. The cerebral
motor cortex sends impulses to the motor neurons, causing stimulation of
respiratory muscles. This bypasses the medullary centers. Holding the breath is
a limited function because the brain stem respiratory centers automatically
reinitiate breathing once CO2 levels in the blood become critical.
1. Describe the medullary respiratory center.
2. Are peripheral chemoreceptors as sensitive to levels of CO2
as they are to levels of oxygen?
3. Differentiate between the central and peripheral
chemoreceptors and their actions.
Related Topics