Trachea
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Respiratory System
The trachea or windpipe is a cylindrical tube about 2 cm in diameter. It is extremely mobile and flexible, with a length of approximately 10–12 cm or 4 inches.
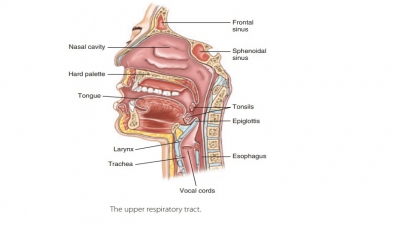
Organization of the Respiratory System
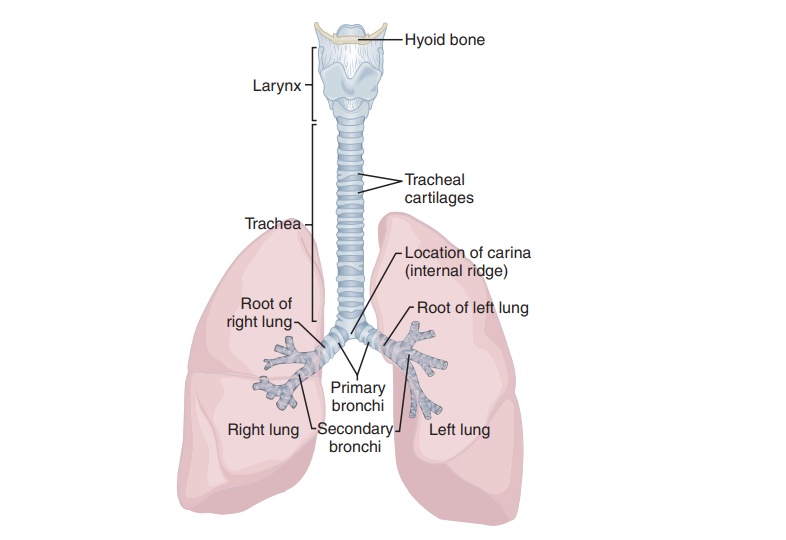
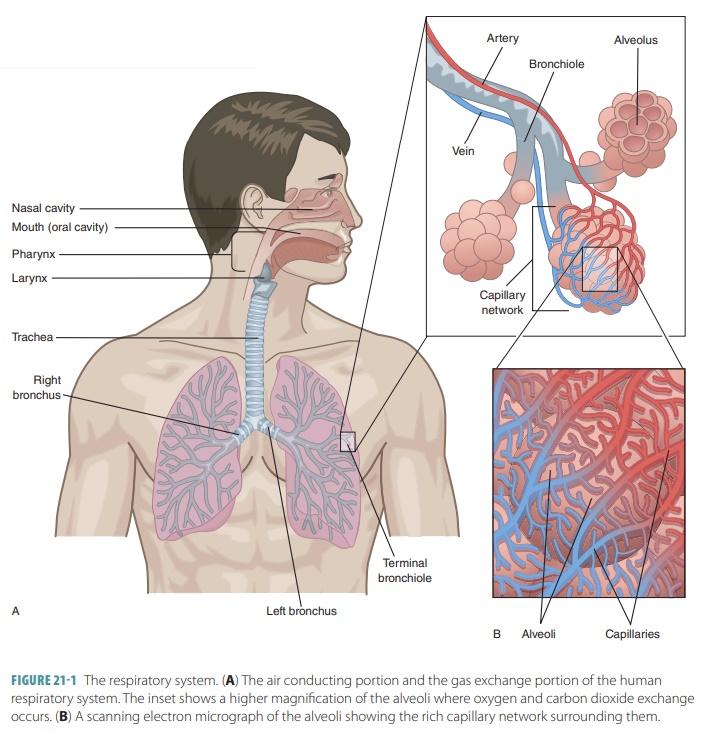
The upper respiratory tract includes the nose, nasal cavity, paranasal sinuses, and pharynx. The lowerrespiratory tract includes the larynx, trachea, and lungs. The lungs contain the bronchi, bronchioles, and alveoli. FIGURE 21-1 shows the structures of the respiratory system.
Trachea
The trachea or windpipe is a cylindrical tube about 2
cm in diameter. It is extremely mobile and flexible, with a length of
approximately 10–12 cm or 4 inches (FIGURE
21- 5). The trachea extends downward from the larynx, anterior to
the esophagus into the medias-tinum of the thoracic cavity, where it splits
into right and left bronchi. The trachea has layers known as the mucosa, submucosa, and adventitia as well as a hya-line
cartilage layer. The ciliated mucosa, like nearby structures, contains goblet
cells in a pseudostratified epithelium. It moves trapped particles up into the
pharynx where they can be swallowed along with mucus. The submucosa is a
connective tissue layer that contains seromucous glands, which help to pro-duce
sheets of mucus. The adventitia is the outermost layer of connective tissue,
encasing the hyaline carti-lage rings of the trachea.
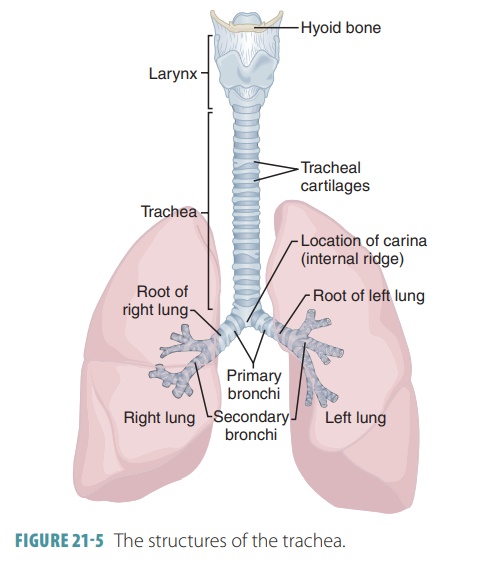
Inside the trachea are about 20 pieces of hyaline cartilage, each shaped like the letter “c.” Their open ends are toward the spine. These rings of cartilage pre-vent the trachea from collapsing. The soft tissue near the back of each ring allows the esophagus to expand as food moves toward the stomach. The open poste-rior parts of these rings of cartilage are connected by smooth muscles in the trachealis as well as by soft con-nective tissues. When the trachealis muscle contracts, the diameter of the trachea increases and expired air is caused to rush upward with great force from the lungs. This helps to expel mucus when coughing, at speeds of approximately 100 miles per hour. A cartilage struc-ture called the carina projects posteriorly from the final tracheal cartilage. This is the point where the tra-chea branches into the two primary bronchi.
Conducting Zone Structures
The structures of the conducting
zone include all respi-ratory passageways except for those that make up the
respiratory zone. The conducting zone structures are relatively rigid and the
organs within function to clean, humidify, and warm the incoming air.
There-fore, when this air reaches the lungs, it contains less dust, bacteria,
and other irritants than when it entered the nose and has become warm and damp.
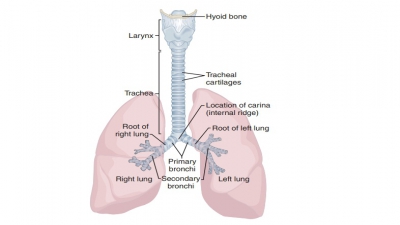
The trachea divides into the right main bronchi and the left
main bronchi, also known as primary
bronchi. Both are found at the level of T7when a personis standing.
The bronchi run obliquely in the medias-tinum. They then move downward into the
hilum or medial depression of the lungs. The left main bronchus is thinner,
longer, and less vertical than the right main bronchus. It is more common for a
foreign object to be inhaled and stuck in the right main bronchus because of
its size, shape, and position.
Branched airways leading from the trachea to the alveoli
make up the bronchial
tree. These branches begin with the right and left primary bronchi near the level of the fifth
thoracic vertebra. Each primary bronchus divides into a secondary bronchus,
then into tertiary bronchi, and even
finer tubes. The right bronchus or bronchus
dexter is wider, shorter, and more vertical than the left bronchus
or bronchussinister.
The right bronchus branches off to theupper lobe of the right lung. This branch
is called the eparterial branch because it arises above the right pulmonary
artery. It then passes below the artery at the hyparterial branch and divides
into two branches for the middle and lower lobes. The left bronchus has no
eparterial branch because there is no third lobe in the left lung. Bronchi have
less cartilage than the tra-chea and bronchioles have no cartilage. Smaller and
smaller respiratory tubes have smooth muscle instead of cartilage.
Bronchioles
are smaller tubes that continue todivide and include terminal
bronchioles. The alveoli provide a large surface of epithelial cells that allow
easy exchange of gases. Oxygen diffuses from the alveoli into the capillaries
and CO2 diffuses from the blood into the alveoli. From each tertiary
bron-chus, about 6,500 terminal bronchioles arise. The lumen of each terminal
bronchiole is only between 0.3 and 0.5 millimeters in width. The bronchiole
walls have no cartilage and are mostly made up of smooth muscle. When the
bronchioles change in diameter, they control resistance to airflow and
distribution of air inside the lungs.
Diameter of the bronchioles is controlled by the autonomic
nervous system, accomplished by regulating smooth muscle activity. Bronchodilation is caused by sympathetic
activation, and airway diameters enlarge. Bronchoconstriction
is caused by parasympatheticactivation, and airway diameters are reduced.
Bron-choconstriction also occurs in anaphylaxis and other allergic reactions, a
response to histamine released by basophils and activated mast cells.
Both bronchodilation and bronchoconstriction adjust
resistance to airflow, and direct airflow to or from certain areas of the
respiratory exchange sur-faces. When there is tension of the smooth muscles,
the bronchiole mucosa usually forms a series of folds, limiting airflow. In
conditions such as asthma, excessive
stimulation can nearly totally prevent airflow along the terminal bronchioles.
Respiratory Zone Structures
The respiratory zone
is where actual gas exchange occurs. It is made up of microscopic structures,
which include the respiratory
bronchioles, alveolarducts,
and alveoli.
The alveoli are thin-walled airsacs. The respiratory zone starts at the point
of the ter-minal bronchioles feeding into the respiratory bron-chioles inside the lungs. Scattered alveoli
protrudefrom the respiratory bronchioles, which also lead into twisting and
turning alveolar ducts. The walls of
the alveolar ducts are completely made up of diffuse rings of connective tissue
fibers, alveoli, and smooth muscle cells. The ducts lead to alveolar sacs or alveolar sac-cules, which are terminal clusters of alveoli.
The alveoli are not the same as the alveolar sacs. The
alveoli are the actual sites of gas exchange. The alveolar sacs resemble
bunches of grapes, with the alveoli being the individual grape-like structures.
There are approximately 300 million alveoli in the lungs, all of them filled
with gas. They make up most of the body’s lung volume, creating a huge surface
area for gas exchange. The alveoli are what give the lungs their open and
spongy appearance. Each alveolus has an extensive capillary network. The
capillaries are sur-rounded by a network of elastic fibers that help main-tain positions
of the alveoli and bronchioles. When the fibers recoil during exhalation, the
size of the alve-oli is reduced, which helps to push air out of the lungs.
In each alveolus, the walls are mostly made up of one layer
of simple squamous epithelial cells, also called type I alveolar cells. These are surrounded by a thin
respiratory basement membrane. The alveolar walls are 15 times thinner than one
sheet of paper. There are also scattered, cuboidal type II alveolar cells, which are also calledseptal cells. These secretesurfactant, an oily substance containing
phospholip-ids and proteins, which coats the alveolar surfaces that are exposed
to gas. Surfactant forms a superfi-cial coating over a thin H2O
layer. The type II cells also secrete many antimicrobial proteins, needed for
innate immunity (FIGURE
21-6). Dust
cells, also known as alveolar
macrophages , patrol the sur-face of the alveolar
epithelium and phagocytize any particles that have not already been “caught” by
other methods.
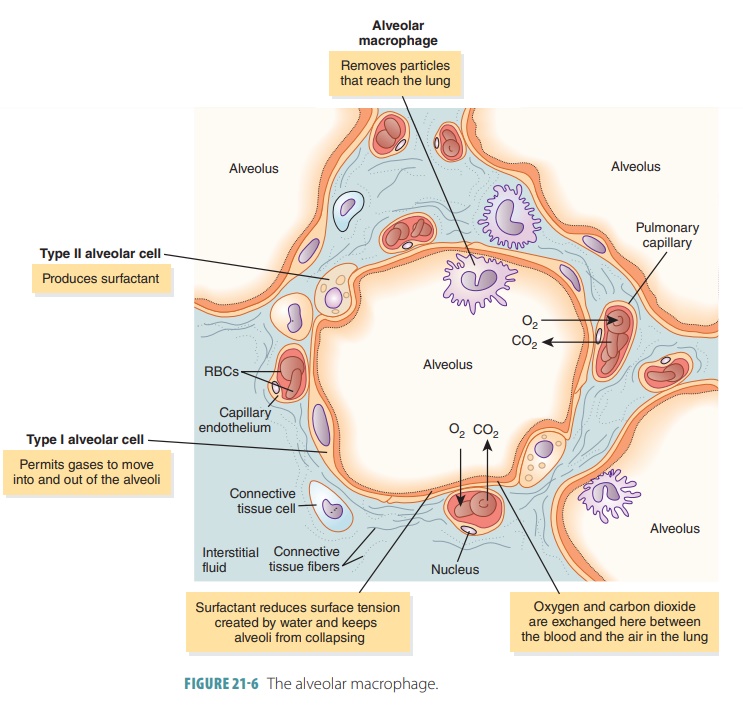
Surfactant is important in keeping the alveoli open and
reduces surface tension in the liquid that coats the alveolar surfaces. If
there were no surfac-tant, surface tension would collapse the alveoli.
Sur-factant forms a thin surface layer, interactive with H2O
molecules, to reduce surface tension and keep the alveoli open.
If the type II alveolar cells do not produce enough
surfactant because of injury or genetic abnormalities, respiration is
difficult. After every exhalation, the alve-oli collapse. This means that each
inhalation must be strong enough to reopen the alveoli. The individual will
soon be exhausted by these efforts. This condition is called respiratory distress syndrome.
At the respiratory membrane, there is a tiny distance separating the alveolar air and blood. This distance averages about 0.5 micrometer, but can be as small as 0.1 micrometer. Diffusion occurs quickly across the respiratory membrane since the distance is tiny, and the oxygen and CO2 molecules are small and lipid-soluble. Oxygen and CO2 are not prevented by the plasma membranes of the epithelial and endo-thelial cells from moving between the alveolar air and blood.
Blood Supply to the Lungs
The lung tissue is nourished by a circuit supply-ing the
respiratory portion and one perfusing the conducting portion. Blood from the
pulmo-nary circuit arteries is received by the respiratory exchange surfaces.
Deoxygenated blood is carried by the pulmonary arteries, which enter the lungs at the hilum.
They branch with the bronchi as they approach the lung lobules. Each lobule
receives one arteriole and one venule. A network of capil-laries surrounds
every alveolus and is part of the respiratory membrane. From the alveolar
capillar-ies, oxygen-rich blood moves through the pulmo-nary venules. It enters
the pulmonary veins, which deliver this blood to the left atrium.
While providing for gas exchange, the endo-thelial cells of
the alveolar capillaries are also the main source of angiotensin- converting enzyme(ACE).
This enzyme converts circulating angioten-sin I to angiotensin II. The enzyme
is important in the regulation of blood volume and pressure. The conducting
passageways of the lungs receive oxy-gen and nutrients from capillaries that
are supplied by the bronchial arteries, which are branches of the thoracic
aorta. Venous blood from these capillar-ies is emptied into bronchial veins or
anastomoses. It then empties into the pulmonary veins. Outside blood flow
bypasses the remainder of the systemic circuit. It dilutes oxygenated blood
that is leaving the alveoli.
In the pulmonary circuit, blood pressure is usually low,
about 30 mm Hg or less. The pulmonary vessels can, therefore, be easily blocked
by masses of fat, small blood clots or air bubbles inside the pulmonary
arter-ies. Since the lungs receive all the cardiac output, any objects moving
through the blood will likely become trapped in the networks of pulmonary
arteries or capillaries. Tiny blood clots are occasionally formed in the
veins. They are usually trapped inside the pul-monary capillaries where they
quickly dissolve. Large emboli are, however, much more dangerous. Blood flow to
a group of alveoli or lobules is stopped when a branch of a pulmonary artery
becomes blocked. This condition is called a pulmonary embolism.
Innervation of the Lungs
Parasympathetic and sympathetic motor fibers along with
visceral sensory fibers innervate the lungs. The visceral sensory fibers enter
each lung through the pulmonary
plexus, which is located on each lung root, and run along the
bronchial tubes and lung blood vessels. The parasympathetic motor fibers
constrict the air tubes (bronchoconstriction),
whereas the sympathetic fibers cause them to dilate (bronchodilation).
Related Topics