Functional Classifications of Joints
| Home | | Anatomy and Physiology | | Anatomy and Physiology Health Education (APHE) |Chapter: Anatomy and Physiology for Health Professionals: Support and Movement: Articulations
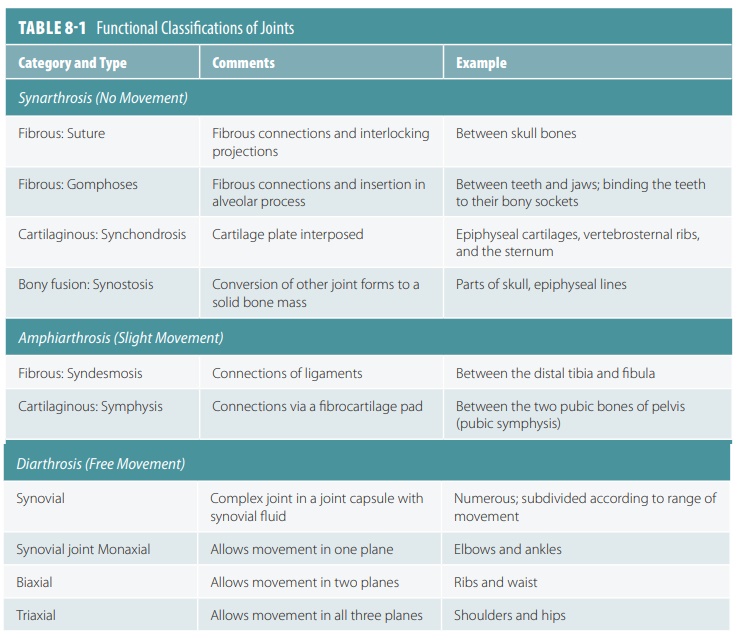
Joints are functionally classified as immovable (synarthrotic), slightly movable (amphiarthrotic), or freely movable (diarthrotic).
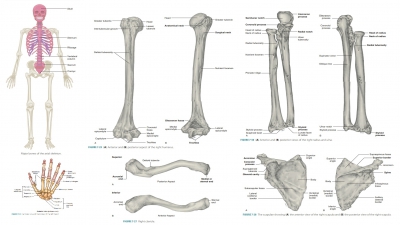
Classifications of Joints
Joints are functionally classified as immovable (synarthrotic), slightly movable (amphiarthrotic), or freely movable (diarthrotic). Less movable joints usually have more stability. They can also be structurally grouped according to the type of tissue binding them at their junctions such as fibrous, carti-laginous, and synovial joints. In general, fibrous joints are immovable, whereas synovial joints are freely movable. Cartilaginous joints may be either rigid or slightly movable. TABLE 8-1 shows functional classifications of joints.
1. List the three types of joints as classified by their degrees of movement.
2. Compare amphiarthrotic with synarthrotic joints.
Fibrous Joints
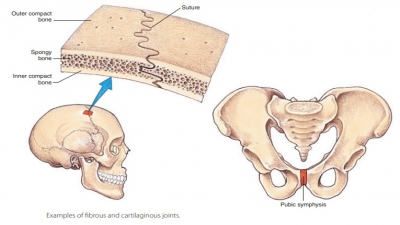
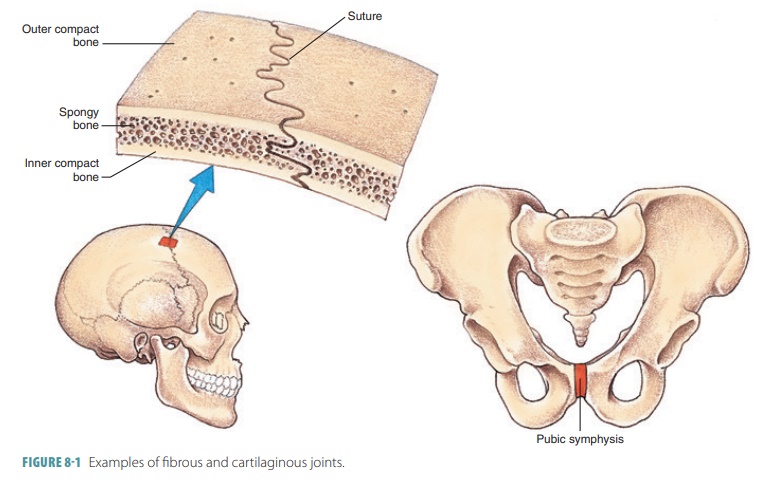
Lying between bones that are in close contact with each other, fibrous joints are joined by a thin, dense connective tissue (FIGURE 8-1). They have no actual joint cavity. An example of a fibrous joint is a suture between flat bones of the skull. No real movement takes place in most fibrous joints, making them synar-throtic in classification. Those with limited movement (amphiarthrotic) include the joint between the distal tibia and fibula. The amount of movement they have depends on the length of the connective tissue fibers that unite the bones. There are three types of fibrous joints: sutures, syndesmoses, and gomphoses.
Sutures
Sutures are seams that occur only between the bones of the skull. They have waved and articulated bone edges that interlock. Each junction is totally filled by a tiny amount of extremely short connective tissue fibers. These fibers are continuous with the periosteum, creat-ing rigid structures joining the bones together. However, they also allow the skull to expand during childhood, when the brain is growing. Closed sutures, during brain growth, are better described as synostoses. The immo-bility of the sutures helps to protect the brain.
Syndesmoses
In syndesmoses, ligaments connect the bones and the connecting fibers are longer than those found in sutures. The varied lengths of these fibers control the amount of movement that can occur. Syndesmoses with shorter fibers have little or no allowed “give” (movement), for example, the ligament connecting the distal ends of the fibula and tibia. When they are longer, more movement is possible, for example, the interosseous membrane (similar to a ligament) that connects the ulna and radius.
Gomphoses
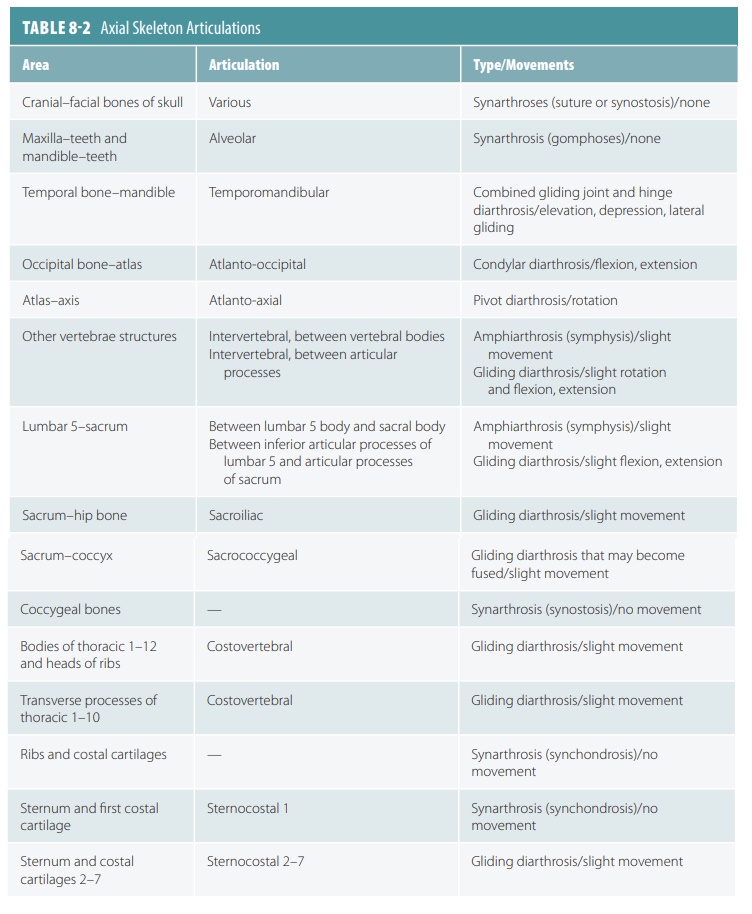
Gomphoses are fibrous joints with a peg-in-socket structure. In the human body, gomphoses are only exemplified by the articulation of the teeth in their alveolar sockets. The singular term gomphosis refers to how the teeth are embedded in their socket (as if they were hammered in) . In gomphoses, the fibrous connects are the short periodontal ligaments. Articulations of the axial skeleton are described in TABLE 8-2.
Cartilaginous Joints
Connected by hyaline cartilage or fibrocartilage, cartilaginous joints include those that separate the vertebrae. Each intervertebral disc is an example of a cartilaginous joint and has slight flexibility. Cartilag-inous joints also lack a joint cavity. The two types of cartilaginous joints are synchondroses and symphyses.
Synchondroses
Synchondroses are plates or bars of hyaline cartilage uniting the bones. Nearly all synchondroses are synarthrotic. In children, the best example of synchondroses is the epiphyseal plates in the long bones. These plates are temporary joints, eventually becoming synostoses. The immovable joint between the manubrium of the sternum and the first rib’s cos-tal cartilage is another example.
Symphyses
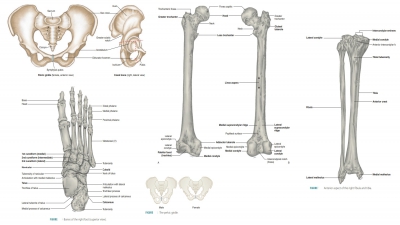
Symphyses are joints where fibrocartilage unites bones (Figure 8-1). Fibrocartilage acts as a shock absorber because of its ability to be compressed and then recover its original shape. A limited amount of movement at the joint is allowed. Hyaline cartilage is also present in symphyses, as articular cartilage on bony surfaces. Symphyses are amphiarthrotic joints allowing flexibility but maintaining strength. Exam-ples include the pubic symphysis of the pelvis and the symphyses of the intervertebral joints.
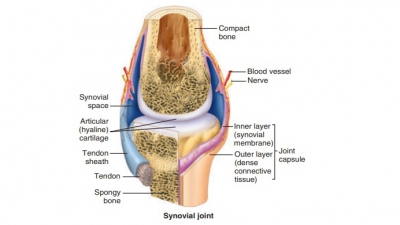
Synovial Joints
These joints allow free movement and are referred to as diarthrotic. They are more complex than other types of joints. Synovial joints have outer layers of ligaments (joint capsules) and inner linings of synovial membrane that secrete synovial fluid, which lubricates these joints (FIGURE 8-2). Some synovial joints have shock-absorbing fibrocartilage pads called menisci. They may also have fluid-filled sacs (bursae), commonly located between tendons and underly-ing bony prominences such as in the knee or elbow. The synovial fluid lubricating these joints allows for great freedom of movement. All synovial joints are freely moving diarthroses. Most joints of the body and nearly all joints of the limbs are synovial joints.
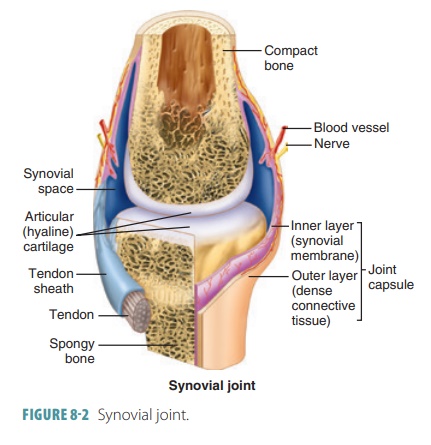
Fat pads are localized adipose tissue masses that are covered by a synovial membrane layer. The six character-istics of synovial joints are:
■■ Articular cartilage: This is made up of smooth hyaline cartilage covering opposing bone surfaces. Although only one millimeter or thinner across, articular cartilage absorbs compression and helps to keep bone ends from being crushed.
■■ Articular cavity: This is a potential space containing a small amount of synovial fluid.
■■ Articular capsule: This two-layered structure that encloses the joint cavity has a tough outer fibrous layer made up of dense irregular connective tissue, which is continuous with the periostea of articulating bones. The capsule strengthens the joint and ensures the bones are not pulled apart. Each joint capsule’s inner layer is known as the synovial membrane, made of loose connective tissue that lines the fibrous layer’s internal portion and covers all internal surfaces of joints that are not covered with hyaline cartilage. The synovial membrane manufactures the synovial fluid.
■■ Synovial fluid: This slippery liquid found in all free spaces inside the joint capsule is mostly syn-thesized by filtration from blood in the synovial also found inside articular cartilages as a slippery film. It bears weight, reducing friction between cartilages. Without it, joint surfaces would be destroyed from use. When a joint is compressed, the fluid is forced out of the cartilages. As joint pressure is relieved, it flows back into the articular cartilages quickly. This process is called weeping lubrication, which also provides nourishment to the cells of the joint cartilage. Synovial fluid also has phagocytic cells that patrol the joint cavity for microbes and cell debris.
■■ Reinforcing ligaments: These are band-like acces-sory structures that reinforce and strengthen syno-vial joints. They are primarily capsular ligaments (actually, thicker parts of the fibrous layer). They are distinct from and remain outside the capsule (extracapsular ligaments) or remain deep to it (intracapsular ligaments). The intracapsular lig-aments do not actually lie within the joint cavity because they are covered with synovial membrane. The term double-jointed actually means a person’s joint capsules and ligaments are looser, with more ability to stretch, than those of the average person.
■■ Nerves and blood vessels: Plentiful in synovial joints, sensory nerve fibers innervate the joint cap-sule, whereas most of the blood vessels supply the synovial membrane. Some sensory nerve fibers detect pain, but most regulate the joint’s position and stretching ability. Therefore, these fibers allow the nervous system to monitor body posture and movements. Extensive capillary beds produce the blood filtrate, which is the basis of synovial fluid Synovial joints sometimes have other structural components. For example, the knee and hip joints have fatty pads between the fibrous layer and the synovial membrane or bone. These add extra cushioning. Other synovial joints have fibrocartilage wedges or discs that separate articular surfaces (these menisci or articular discs were introduced earlier). They extend in from the articular capsule, dividing (or partially dividing) the synovial cavity in half. Articular discs help articu-lating bone ends to fit better, stabilizing the joint and lessening friction on the joint surfaces. Articular discs occur in the knees, jaw, and other areas.
Bursae and Tendon Sheaths
The bursae and tendon sheaths are closely related to the synovial joints. They act similar to lubricated ball bearings, reducing friction during joint activ-ity between nearby structures. Bursae are flat fibrous sacs that have synovial membranes lining them. They contain a thin film of synovial fluid and are located where bones, ligaments, muscles, skin, or tendons rub together. A tendon sheath can be understood as a lengthened bursae wrapping totally around a tendon that is subjected to friction. They are common in areas such as the wrist, where several tendons are tightly crowded inside narrow canals.
Joints must be stabilized to avoid becoming dislocated during stretching and compression. Joint stability relies on articular surface shapes, number and position of ligaments, and also on muscle tone. Artic-ular surfaces actually play just a minor role. When they are larger and well fitting or when sockets are deep, joint stability is greatly improved. For example, the hip’s ball and socket joint is very stable because of the shape of its articular surfaces.
Bones are united, and excessive or undesirable motions are prevented by the capsules and ligaments of synovial joints. Generally, the more ligaments that exist, the stronger the joint. Sometimes, excessive ten-sion on the ligaments causes them to stretch, which is a condition that remains. Ligaments stretch approx-imately 6% of their length, until they break. When a joint is mostly braced by ligaments and this occurs, the joint becomes highly unstable.
Muscle tendons crossing joints are often the most important factors concerning stability. Muscle tone keeps these tendons tense. It means that the muscle, when relaxed, has low levels of contractile activity. This keeps muscles healthy and ready for stimulation. Muscle tone is vital for reinforcing areas such as the foot arches and the joints of the knees and shoul-ders. Articulations of the appendicular skeleton are described in TABLE 8-3.

Types of Synovial Joints
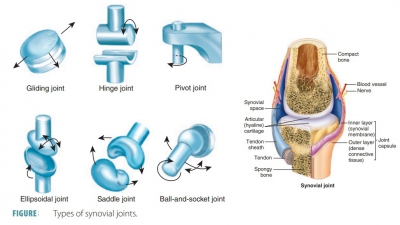
Synovial joints are not all identical. There are six further subdivisions of synovial joints: gliding, hinge, pivot, ellipsoidal, saddle, and ball-and-socket joints.
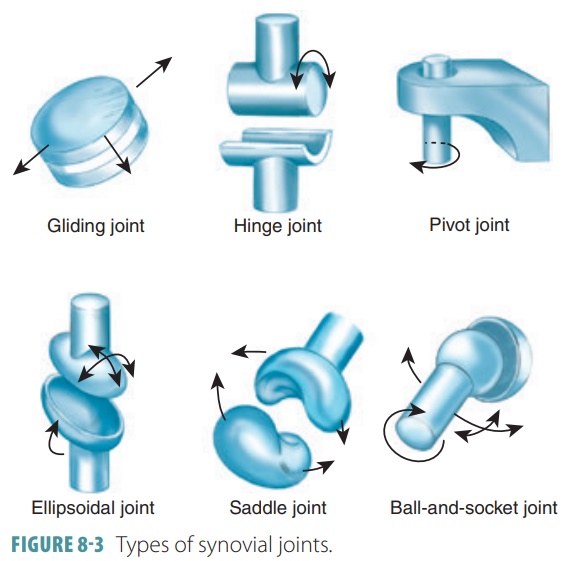
Gliding Joints
Gliding joints have nonaxial movement that involves linear gliding and flat, articular surfaces. For exam-ple, the intercarpal joints, intertarsal joints, sacroil-iac joints, and the joints between vertebral articular surfaces.
Hinge Joints
Hinge joints have uniaxial movement that involves flexion and extension along a medial/lateral axis. They also have cylinders and troughs. For example, the elbow joints and interphalangeal joints.
Pivot Joints
Pivot joints have uniaxial movement that involves rotation around a vertical axis. They have bone and ligament sleeves as well as rounded bones (axles). For example, the proximal radioulnar joints and the atlan-toaxial joint.
Ellipsoidal Joints
Ellipsoidal joints have biaxial movement that involves adduction and abduction around an anterior/ posterior axis as well as flexion and extension around a medial/lateral axis. Their articular surfaces are oval-shaped. For example, the metacarpophalangeal (knuckle) joints, radiocarpal joints, and wrist joints.
Saddle Joints
Saddle joints have biaxial movement that involves flexion and extension as well as adduction and abduc-tion. These joints function around the same type of axis configurations as condylar joints. Articular sur-faces are both concave and convex. For example, the carpometacarpal joints of the thumbs.
Ball-and-Socket Joints
Ball-and-socket joints have multiaxial movement that involves rotation, adduction, abduction, flexion, and extension. These joints use vertical, anterior/ posterior, and medial/lateral types of axis structures, with spherical heads in cup-like sockets. For example, the shoulder and hip joints. Types of synovial joints are shown in FIGURE 8-3.
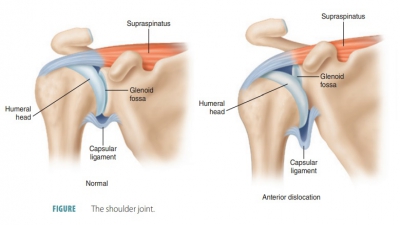
Shoulder Joints
The shoulder joints are the most freely movable joints of the body, but they lack stability. They are ball-and-socket joints. The head of the humerus is large and hemispherical. It fits in the glenoid cavity of the scapula, which is shallow and small (FIGURE 8-4). This cavity is made slightly deeper by a fibrocartilage rim (the glenoid labrum). Still, it is only about one -third the size of the humeral head, which means the shoulder joint is highly unstable. A shoulder separation is an injury involving partial or complete dislocation of the acromioclavicular joint.
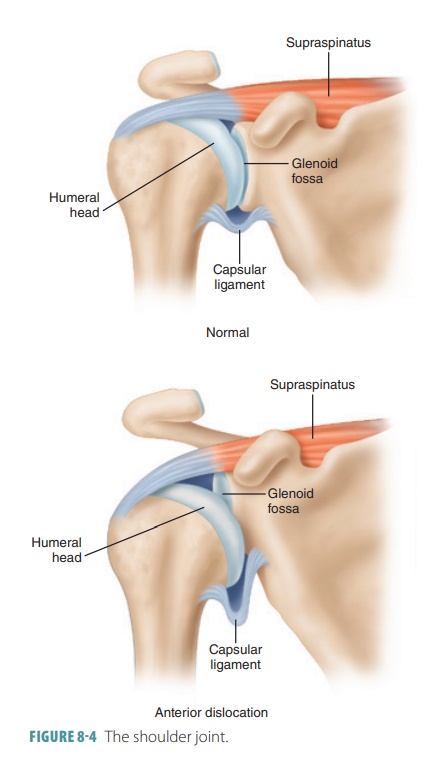
The joint cavity is enclosed by an extremely loose, thin articular capsule. It runs from the margin of the glenoid cavity to the anatomical neck of the humerus. Only a few ligaments reinforce the shoulder joint, and these are found mostly on its anterior aspect. The supe-rior coracohumeral ligament is the thickest area of the capsule. It helps to support the weight of the arm. The front of the capsule is only slightly strengthened by three glenohumeral ligaments. These are absent in some individuals. Most of the stability of the shoulder joint comes from muscle tendons that cross the joint. The primary stabilizing structure is the tendon of the long head of the arm’s biceps brachii muscle. This tendon secures the head of the humerus against the glenoid cavity. It is attached to the glenoid labrum’s superior margin and travels through the shoulder joint cavity. It then continues within the intertubercular sulcus of the humerus.
Associated muscles (the subscapularis, infraspi-natus, supraspinatus, and teres minor) and a total of four other tendons comprise the rotator cuff, which encircles the shoulder joint. The rotator cuff blends with the articular capsule. If the arm is strongly circumducted, the rotator cuff can be stretched severely, which often occurs in athletes who pitch (such as those in baseball or softball). Instability of the shoulder joint also results in frequent disloca-tions. Usually, the humerus dislocates in the forward, downward direction because its reinforcements are weakest anteriorly and inferiorly.
Elbow Joints
The elbow joints allow only flexion and extension and are stable hinge joints that operate very smoothly. The radius and ulna bones both articulate inside each elbow joint with the condyles of the humerus. The hinge of the elbow joint is formed by the tight gripping of the troch-lea by the trochlear notch of the ulna. Joint stabilization is provided by this structure. The articular capsule is rel-atively loose. It extends inferiorly from the humerus to the radius and ulna and to the annular ligament that surrounds the head of the radius. The humeroulnar joint is the largest and strongest articulation at the elbow.
The articular capsule of the elbow joint is thin both anteriorly and posteriorly. Two strong capsular ligaments restrict horizontal movements: the medial ulnar collateral ligament and the triangular radial collateral ligament on the lateral side. Several arm muscle ligaments also cross the elbow joint to make it more secure. These are the tendons of the biceps and tri-ceps. The radius has less activity in movements of the elbow, but its head rotates inside the annular ligament during both pronation and supination of the forearm.
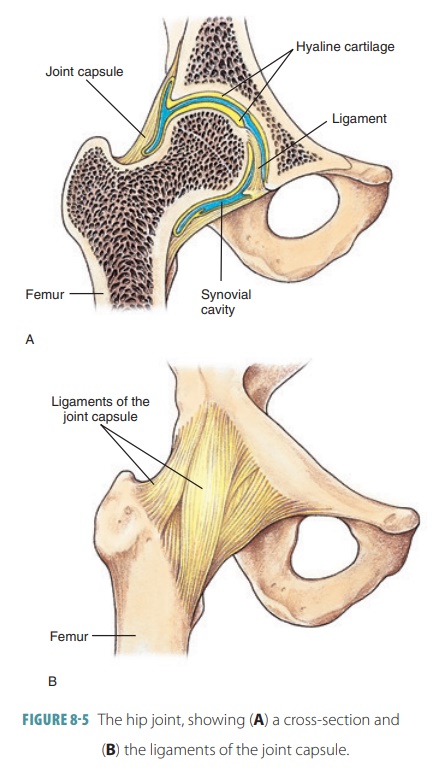
Hip Joints
The hip joints are also known as the coxal joints. They are ball-and-socket joints with less range than those of the shoulder. Although widely ranging movements are possible, they are limited by the deep hip sockets and strong ligaments. Each hip joint is formed by the artic-ulation of the femur’s spherical head with the hip bone’s acetabulum and its deeply cupped position (FIGURE 8-5). A circular rim of fibrocartilage called the acetabular labrum increases the depth of the acetabulum. Hip joint dislocations are rare because the articular surfaces fit tightly together. The labrum’s diameter is less than that of the head of the femur, however.
Each hip joint is completely enclosed by its thick articular capsule, which extends from the rim of the ace-tabulum to the femur neck. The capsule is reinforced by the iliofemoral ligament, pubofemoral ligament, and ischiofemoral ligament. The iliofemoral ligament lies anteriorly and is very strong, with a V-shape. The pubofemoral ligament is a triangular thickening of the inferior area of the capsule. The ischiofemoral ligament spirals posteriorly. All three ligaments have an arrange-ment that causes a screw-like turning motion of the femur head into the acetabulum when a person stands up straight. They provide increased joint stability.
The ligamentum teres, which is the ligament of the femur head, is the flattened intracapsular band connecting the femur head to the acetabulum’s lower edge. During most movements of the hip, it is slack. It is not important in joint stabilization, but contains an artery supplying the head of the femur. When the artery is damaged, severe hip joint arthritis may develop. Stability of the hip joint comes from the deep socket that strongly encloses the femur head, strong capsular ligaments, thick hip and thigh muscles sur-rounding it, and muscle tendons crossing it.
Knee Joints
The knee joint has a single joint cavity, yet is the most complex joint in the body ( FIGURE 8-6). It is actually made up of an intermediate joint between the patella and lower femur and lateral and medial joints, collec-tively known as the tibiofemoral joints. These joints lie between the femoral condyles above and the semi-lunar cartilages (C-shaped menisci) of the tibia below. The semilunar cartilages deepen the tibial articular sur-faces, which are otherwise shallow. They absorb shock to the knee joint and also prevent horizontal rocking of the femur on the tibia. Unfortunately, the semilunar cartilages are often completely torn because they are only attached at their outer margins. The menisci are damaged most commonly in athletic knee injuries.
Flexion and extension is allowed by the hinge-like tibiofemoral joint. In actuality, it is a bicondylar joint, with some rotation occurring when the knee is slightly flexed or when it is extending. A fully extended knee cannot rock horizontally or rotate without difficulty because of strong ligament and menisci resistance. The patella glides across the femur’s distal end during knee flexion because the femoropatellar joint is a plane joint.
The knee joint is the only articulation that has a cavity partially enclosed by a capsule. This capsule is thin and present only on the posterior aspects and sides of the knee. It covers most of the femoral and tibial condyles. It is absent anteriorly, and here, there are three broad ligaments running from the patella to the tibia below: the patellar, medial, and lateral patel-lar retinacula . They merge with the articular capsule on each side. Two of them (the patellar ligament and the lateral patellar retinacula) are continuations of the tendon from the quadriceps muscle in the ante-rior thigh. The patellar ligament is used to test the knee-jerk reflex.
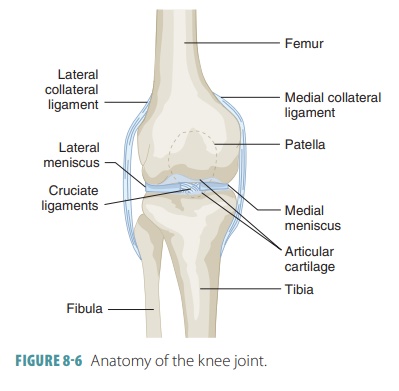
The knee joint’s synovial cavity is also complex, with various bursae. The subcutaneous prepatellar bursa is an example of a bursa that is often injured by trauma to the anterior knee. The knee joint capsule is strengthened and stabilized by all three types of joint ligaments. Two of these types (capsular and extracap-sular) help to prevent hyperextension of the knee. They are tightly stretched when the knee is extended. When the knee is extended, the extracapsular fibu-lar and tibial collateral ligaments are crucial to pre-vent lateral or medial rotation. The tibial collateral ligament is wide and flat, running from the femur’s medial epicondyle to the tibial shaft’s medial condyle. This ligament is fused to the medial meniscus. The posterior aspect of the knee joint is partially stabilized by the oblique popliteal ligament, which is part of the tendon of the semimembranosus muscle. It fuses with the joint capsule. The joint capsule is reinforced posteriorly by the arcuate popliteal ligament, which has a superior arc, from the head of the fibula over the popliteus muscle.
In the notch between the femoral condyles, the intracapsular ligaments (cruciate ligaments) cross each other to form an “X.” They provide restraint against anterior–posterior displacement of the articular sur-faces. These ligaments also secure the articulating bones during standing. They are in the joint capsule but outside the synovial cavity. Therefore, the intra-capsular ligaments are nearly covered by synovial membrane and run superiorly to the femur. They are named for their tibial attachment site.
The anterior cruciate ligament is attached to the tibia’s anterior intercondylar area and passes upward, laterally, and posteriorly to attach to the femur. Its actual point of attachment is the medial side of the femur’s lateral condyle. The anterior cruciate ligament prevents the tibia from sliding for-ward on the femur, controlling hyperextension of the knee. It is tight during knee extension and slightly relaxed during knee flexion. The posterior cruciate ligament has more strength and is attached to the tibia’s posterior intercondylar area. This ligament passes superiorly, medially, and anteriorly, attaching to the lateral side of the medial condyle of the femur. It prevents forward sliding of the femur or backward displacement of the tibia.
Many muscle tendons reinforce the knee capsule. Muscle strength and tone protect the knee from injury. This is especially true of the tendon of the semimem-branous muscle (posteriorly) and the tendons of the quadriceps muscles in the anterior thigh.
When standing, the knees “lock in” to provide steady support. As a person rises from a sitting to a standing position, the wheel-like femoral condyles roll across the tibial condyles as the flexed leg begins to extend at the knee. The lateral femoral condyle stops rolling before the medial condyle stops. Therefore, the femur rotates medially on the tibia, followed by twisting and tightening of the collateral and cruciate ligaments of the knee. The menisci become compressed. Tension present in the ligaments makes the joint become rigid. It cannot be flexed once more until it is “unlocked,” which is accomplished by the popliteus muscle. This muscle causes the ligaments to become slack and untwisted by rotating the femur laterally on the tibia.
Temporomandibular Joints
Each temporomandibular joint (TMJ) in the jaw is a modified hinge joint. Lying just anterior to the ear, the condylar process of the mandible is articulated with the inferior surface of the squamous area of the temporal bone. The condylar process is shaped like an egg. The articular sur-face of the temporal bone, however, has a more complicated shape. Anteriorly, it forms the dense
knoblike structure known as the articular tubercle. Posteriorly, it forms the concave-shaped mandib-ular fossa. The lateral aspect of the loose articular capsule encloses the TMJ and thickens to form the lateral ligament. Inside the capsule, the articular disc divides the synovial cavity into superior and inferiorsections.
The (TMJ) allows two types of movement. Its concave inferior disc surface receives the mandible’s condylar process. This allows the hinge-like move-ment of depressing and elevating the mandible as the mouth is opened and closed. The second type of movement occurs as the superior disc surface glides anteriorly with the condylar process as the mouth is widely opened. This anterior movement braces the condylar process against the articular tubercle. Therefore, the mandible cannot move through the thin “roof ” of the mandibular fossa when biting is required of hard foods. The superior section allows the joint to glide from side to side. When grinding motions occur, the posterior teeth are drawn into occlusion, and the mandible moves side to side, a movement known as lateral excursion. This lateral movement of the jaw only occurs in humans and other mammals.