Mechanisms of Pharmacokinetic Drug Interactions
| Home | | Biopharmaceutics and Pharmacokinetics |Chapter: Biopharmaceutics and Pharmacokinetics : Pharmacokinetic Drug Interactions
The three mechanisms by which an interaction can develop are -
Mechanisms of Drug Interactions
The three mechanisms by which an interaction can
develop are —
1. Pharmaceutical Interaction – Also
called as incompatibility, it is a physicochemical interaction that occurs when drugs are mixed in i.v. infusions causing
precipitation or inactivation of active principles, for example, ampicillin,
chlorpromazine and barbiturates interact with dextran in solutions and are
broken down or form chemical complexes.
2. Pharmacokinetic Interactions – These interactions are those in which
the absorption, distribution,
metabolism and/or excretion of the object drug are altered by the precipitant
and hence such interactions are also called as ADME interactions. The
resultant
effect is altered plasma concentration of the object drug. Pharmacokinetic interactions
can thus be classified as –
(i) Absorption interactions – are those where the absorption of the object drug is altered.
The net effect of such an interaction is –
·
Faster or slower drug absorption
·
More, or, less complete drug
absorption.
Major mechanisms of absorption interactions are –
·
Complexation and
·
adsorption. Alteration in GI
·
pH. Alteration in gut motility.
·
Inhibition of GI enzymes.
·
Alteration of GI microflora.
·
Malabsorption syndrome.
(ii) Distribution interactions – are
those where the distribution pattern of the object drug is altered. The major
mechanism for distribution interaction is alteration
in protein-drug binding.
(iii)Metabolism interactions – are those
where the metabolism of the object drug is altered. Mechanisms of metabolism
interactions include –
·
Enzyme induction – increased rate of metabolism
·
Enzyme inhibition – decreased rate of metabolism. It is the most significant interaction in comparison to other
interactions and can be fatal.
(iv) Excretion interactions – are those where the excretion pattern of the object drug is
altered. Major mechanisms of excretion interactions are –
·
Alteration in renal flood flow – e.g. NSAIDs (reduce renal blood flow)
with lithium.
·
Alteration of urine pH – e.g. antacids with amphetamine.
·
Competition for active secretion – e.g. probenicid and penicillin.
·
Forced diuresis.
3. Pharmacodynamic Interactions – are those in which the activity of the
object drug at its site of action is
altered by the precipitant. Such interactions may be direct or indirect.
(i) Direct pharmacodynamic
interaction is the one in which drugs having
similar or opposing pharmacological effects are used concurrently. The
three consequences of direct interactions are –
(a) Antagonism: The interacting drugs have opposing actions, e.g.
acetylcholine and noradrenaline have opposing effects on heart rate.
(b) Addition or Summation: The
interacting drugs have similar actions and the resultant effect is the
sum of individual drug responses, e.g. CNS depressants like sedatives,
hypnotics, etc.
(c) Synergism or Potentiation: It is
enhancement of action of one drug by another, e.g. alcohol enhances the
analgesic activity of aspirin.
(ii) Indirect pharmacodynamic
interactions are situations in which both the object and the precipitant drugs have unrelated effects but the latter in
some way alters the effects of the former, for
example, salicylates decrease the ability of the platelets to aggregate thus impairing the haemostasis if warfarin
induced bleeding occurs.
The resultant effect of all
pharmacodynamic interactions is thus altered drug action without a change in
plasma concentration.
Of the various types of interactions, the pharmacokinetic interactions are most
common and often result in differences in pharmacological effects. Several
examples of such interactions are known but few are clinically significant.
Clinically important effects are precipitated by drugs having low therapeutic
indices, e.g. digoxin or those having poorly defined therapeutic end-points, e.g.
antipsychotics.
The net effect of all pharmacokinetic interactions
is reflected in the altered duration and intensity of pharmacological action of
the drug due to variation in the plasma concentration precipitated by altered
ADME. All factors which influence the ADME of a drug affect its
pharmacokinetics. The same has already been dealt with in sufficient details in
the respective chapters. A summary of some of the important pharmacokinetic
interactions is given in Table 7.1.
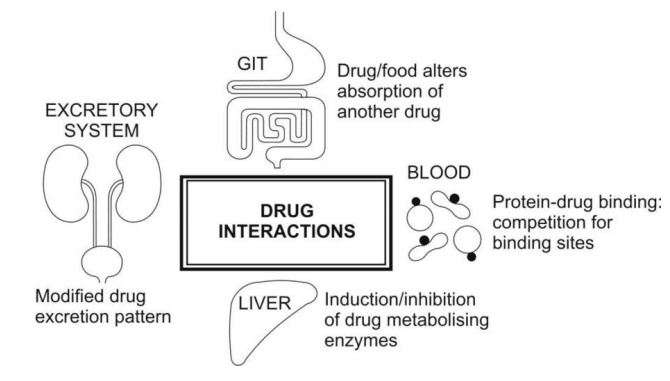
Fig. 7.1. Major sites of pharmacokinetic
interactions
Related Topics
