Devices for pulmonary drug delivery
| Home | | Pharmaceutical Drugs and Dosage | | Pharmaceutical Industrial Management |Chapter: Pharmaceutical Drugs and Dosage: Organ-specific drug delivery
Pulmonary drug delivery almost invariably requires aerosolization of the drug using a device or mechanism that can achieve controlled drug particle formation and delivery.
Devices for
pulmonary drug delivery
Pulmonary
drug delivery almost invariably requires aerosolization of the drug using a device
or mechanism that can achieve controlled drug particle formation and delivery.
Examples of devices that have been used for pulmo-nary delivery include the
following:
1. Metered dose
inhaler:
Pressurized spray is a metered dose inhaler (MDI) that incorporates propellant(s), surfactant(s), and the drug in
either dis-solved or suspended state in its formulation. Pressurized metered
dose inhalers provide constant pressure on the liquid formulation and
con-sistent quantity of drug release on actuation of the valve. The
propel-lants used in these formulations include chlorofluorocarbons (CFCs) and
hydrofluoroalkanes (HFAs). Effective use of an MDI requires patient
coordination of breathing and actuation to provide maximum amount and flow
velocity of air going into the lungs. Drug solubility, vapor pressure, surface
tension, solubility of oxygen/hygroscopicity, and density affect the
effectiveness of drug delivery through the MDIs. MDIs are commonly used for the
delivery of drugs for asthma and chronic obstructive pulmonary diseases (COPD).
2. Nebulizer: The nebulizer uses
an air compressor as a power source instead
of a liquid propellant. Compressed air is brought in contact with an aqueous
solution of the drug in a device. Liquid shearing leads to the formation of
drug droplets that get inhaled by the patient. Droplet size is a key factor in
effective pulmonary delivery of the drug through this route. The droplet size
is typically controlled through the orifice diameter of the baffle, pressure of
the gas, and the density, con-centration, viscosity, surface tension, and flow
rate of the drug solu-tion. Nebulizers are frequently used in applications
where patient’s strong inhalation is not required for effective drug delivery
such as in pediatric or hospitalized patients.
3. Dry powder
inhaler:
The dry powder inhaler (DPI) allows the drug to be formulated in dry state, in which it may be more stable, does
not require the use of a liquid propellant, and also does not require patient
coordination between breathing and actuation. DPIs consist of a sus-pension of
fine particulate drug formulation, which is dispersed by mechanical, pneumatic,
or electrical energy, or by the strength of the vacuum generated by the
patient’s breathing. DPIs have been used to treat diseases such as asthma,
bronchitis, emphysema, and COPD.
Optimization
of particle properties and device parameters can increase drug penetration to
the lungs. For example, simulation results of hydroflu-oroalkane
(HFA)-propelled metered dose inhaler (pMDI) show increased droplet transport
and deposition to the lungs when used with a spacer (Figure
15.1). This study illustrates the impact of a simple spacer in terms of
enhanced droplet percentage reaching the tracheobronchial tree.
For
further discussion and details on the devices used for pulmonary drug delivery,
see Chapter 24.
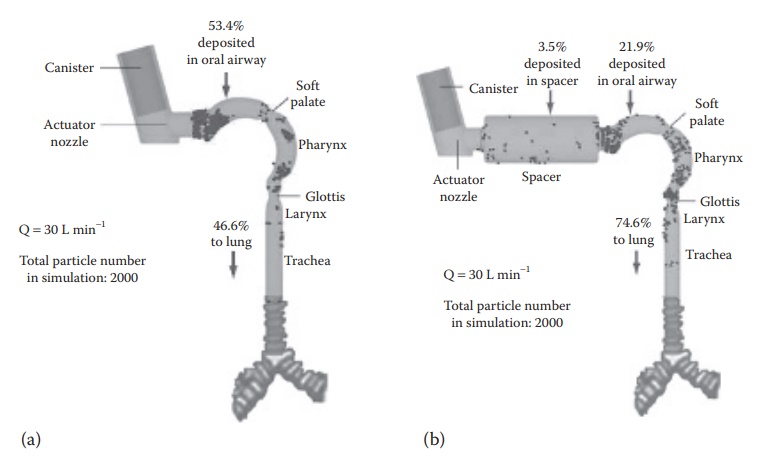
Figure 15.1 Drug delivery to the lung. Role of device in enhanced drug penetration
into the lung. Simulation results of hydrofluoroalkane (HFA)-propelled metered
dose inhaler (pMDI) droplet transport and deposition: (a) without and (b) with
spacer, illustrating the impact of a simple spacer in terms of enhanced droplet
percentage reaching the tracheobronchial tree. Q = Airflow Rate. (Courtesy of
Annual Reviews, Palo Alto, CA.)
Related Topics
