Ocular drug delivery
| Home | | Pharmaceutical Drugs and Dosage | | Pharmaceutical Industrial Management |Chapter: Pharmaceutical Drugs and Dosage: Organ-specific drug delivery
Antibiotics and steroids are the most common classes of drugs typically administered to the eye.
Ocular drug
delivery
Antibiotics
and steroids are the most common classes of drugs typically administered to the
eye. These drugs are administered most commonly through the topical route by
instilling or application to the surface (cornea) of the eye. Nevertheless,
drug delivery is often required for different segments and anatomical regions
of the eye that are difficult to access. Treatment of ocular disorders is
challenging due to anatomical and physiological con-straints of the eye,
including its vascular permeation and sequential presence of both lipophilic
and hydrophilic barriers to drug penetration upon topical administration. In Section 15.6.1.1, we will discuss the structure of
the eye, challenges to drug delivery to the eye, and the approaches that have
been taken to overcome these challenges.
1. Structure of the eye
The
eye is divided into two chambers—commonly known as the anterior chamber and the
posterior chamber (Figure 15.2). The anterior
chamber
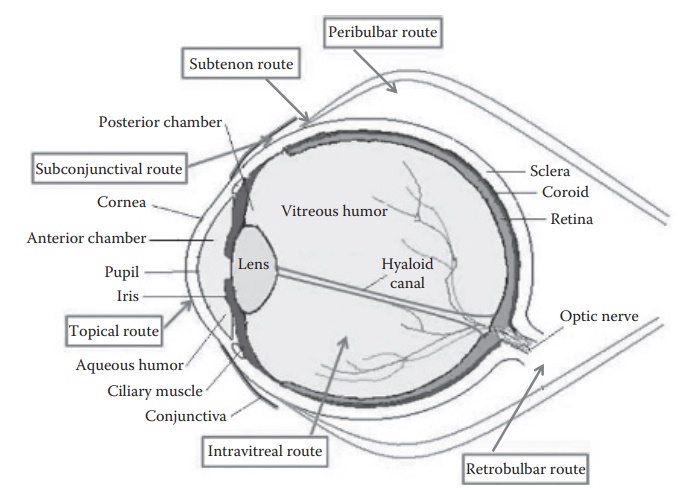
Figure 15.2 Drug delivery to the eye: Structure and schematic representation of
various routes of drug delivery to the eye. (Reproduced from Mishra, G.P. et
al., Recent advances in ocular drug delivery: Role of transporters, receptors,
and nanocarriers, in Narang, A.S., and Mahato, R.I. (Eds.), Targeted Delivery
of Small and Macromolecular Drugs , Boca Raton, FL: CRC Press, Taylor &
Francis Group, pp. 421–453, 2010. With permission.)
The
posterior chamber includes sclera, choroid, vitreous humor, and retina.3 Cornea is the outermost, avascular and transparent
membrane of the eye. The conjunctiva is a clear mucous membrane that covers the
inner part of the eyelid and the visible part of sclera (white part of the eye)
and lubricates the eye by producing mucus and some tears. Aqueous humor lies
between the lens and the cornea. It circulates from the posterior to the
anterior chamber of the eye and through the canal of Schlemm. Impaired outflow
of aqueous humor causes elevated intraocular pressure that leads to permanent
damage of the optic nerve and consequential visual field loss that can progress
to blindness. Retina is a light-sensitive tissue behind the aqueous humor. The
vitreous humor is a hydrogel matrix composed of hyaluronic acid and collagen
fibrils and is located between the retina and the lens.
2. Routes of drug administration into the eye
Depending
on the targeted location of drug action within the various com-ponents and
compartments of the eye, the selection of the site of adminis-tration can play
a key role in drug targeting.
1.
Topical route of
drug administration: Treatment of anterior segment diseases usually utilizes topical route of drug administration.
This route presents challenges such as precorneal tear clearance, limited
conjunctival drug absorption, metabolism by the iris-ciliary body, and
elimination through the canal of Schlemm.
2.
Systemic drug
administration: Systemic drug administration is usu-ally not preferred for
drug delivery to the eye. However, in certain cases, such as the treatment of
glaucoma, administration of drugs, such as acetazolamide, through the systemic
route may be preferred to obviate the drug absorption limitation due to high
intraocular pressure.
3.
Intravitreal
administration:
Intravitreal (IVT) injection is utilized for
the treatment of posterior segment diseases, for example, diabetic
retinopathy, and viral infections, for example, human cytomegalovi-rus (HCMV)
retinitis and endophthalmitis. Direct administration to the vitreous humor
overcomes the blood-retinal barrier (BRB). This route, however, requires
injections in the eye and may cause retinal detachment, which could lead to
vision loss. Thus, prolonged drug release strategies, including prodrugs, have
been utilized to prolong drug residence time in the vitreous humor.
4.
Periocular
administration:
The periocular route of administra-tion provides direct access to the sclera,
and can result in high drug concentration both in the anterior and posterior
segments of the eye. The periocular drug injections could be retrobulbar,
peribulbar, sub-tenon, and subconjunctival, depending on the site of injection.
5.
Retrobulbar
injection:
Direct injection into the retrobulbar space
can be useful for drug delivery into the macular region (highly pig-mented
yellow spot near the center of retina, rich in ganglion cells and responsible
for central vision). This injection can, however, result in damage to the blood
vessels.
6.
Peribulbar injection: The peribulbar
injection can be circumocular, periocular,
periconal, or apical depending on the exact site of injection. This route is
generally utilized for the administration of analgesics.
7.
Subtenon injection: This site of drug
injection can be utilized for drug delivery
to the posterior segment of the eye. The drug is administered into the tenon
space, which is formed by the void between the tenon’s capsule and the sclera.
8.
Subconjunctival
injection: This
periocular route of drug administra-tion can allow up to 500 μL of drug solution to be injected.
This route is utilized for the treatment of both anterior and posterior segment
diseases.
3. Challenges to ocular drug delivery
Topically administered drugs can be eliminated via precorneal tear clear-ance, blinking, and nasolacrimal drainage. This presents challenges to the entry of drug molecules to the anterior segment of the eye (Figure 15.2). Drug delivery to the posterior segment of the eye is challenged by barriers such as inner and outer BRBs and efflux pumps. In addition, the presence of efflux pumps, such as P-glycoprotein (P-gp), multidrug resistance associ-ated proteins (MRPs), and breast cancer resistant protein, also limits the ocular bioavailability of drugs.
For
drugs administered through the topical route, the cornea is the main barrier to
drug absorption. The cornea and the conjunctiva are covered with a thin film,
the tear film, which protects the cornea from dehydration and infection.
Following topical administration, a drug is eliminated from the eye by
nasolacrimal drainage, tear turnover, productive corneal absorp-tion. and
nonproductive conjunctival uptake. The cornea has three ana-tomical parts: (1)
the epithelium, (2) the stroma, and (3) the endothelium. Both the endothelium
and the epithelium have high lipid content, and thus are penetrated by drugs in
their unionized lipid-soluble forms. The stroma lying between these two
structures has high water content. To penetrate the cornea, drugs have to go
through both the lipidic and aqueous anatomical components.
For
drugs injected into the eye, there are two main barriers to ocular drug
adsorption: (a) the blood-aqueous barrier and (b) the blood-retina barrier. The
blood-aqueous barrier is composed of the ciliary epithelium, the epithelium of
the posterior surface of the iris, and blood vessels within the iris. Drugs
enter the aqueous humor at the ciliary epithelium and in the blood vessels.
Many substances are transported out of the vitreous humor at the retinal
surface.
4. Physicochemical characteristics of the drug for ocular absorption
Drug
ionization impacts absorption through the ocular route not only by impacting
drug permeability but also by affecting tear turnover. A pH 5 solution induces
more tear flow than a pH 8 solution. Greater tear turnover can lead to
reduction of concentration gradient in addition to drug loss on blinking.
Transport of both ionized and unionized drugs is less at pH 5.
The
duration of drug action in the eye can be extended by two approaches:
1. Reducing drainage with viscosity-enhancing agents,
suspensions, emulsions, ointments, and polymeric matrices
2. Improving corneal drug penetration with ionophores and
liposomes
5. Approaches for enhancing drug delivery to the eye
Drug
delivery to the eye can utilize multiple mechanisms to overcome the barriers to
drug absorption. These include the modification of physi-cochemical properties
of the drug such as by making prodrugs, targeting natural transporters and
receptors for uptake, inhibition of efflux trans-porters, prolonging the drug
residence time at the site of absorption by using nanoparticles,
microparticles, micelles, and liposomes; or using mucoadhe-sive ocular implants
and hydrogel-based aqueous formulations to achieve relatively constant drug
levels at the target site for a longer duration.
1. Prodrugs: Prodrugs are
chemical entities that are pharmacologically
inactive but can generate an active drug upon absorption through various
chemical bond cleavage mechanisms, such as hydrolysis. Prodrugs can be utilized
for changing the physiochemical properties of a drug, such as aqueous
solubility and lipophilicity, or targeting specific transporters or receptors
expressed on cell membranes. For example, lipophilic acyl ester prodrugs of
acyclovir (ACV) were inves-tigated to allow high drug permeability through
lipophilic membrane. Prodrug hydrolysis to the parent ACV after prodrug
permeation and its transformation to ACV-triphosphate prevent diffusive back
trans-port of the ACV. Amino acid and peptide prodrugs of quinidine and
ganciclovir were investigated to bypass efflux pumps and to target peptide
transporters for drug absorption.
2. Permeability and efflux pump modification: Formulation
strategies for topically administered
drugs that modify drug permeability and/or inhibit P-gp mediated efflux can be
utilized to improve drug perme-ation into the eye. Several surfactants (such as
d-alpha-tocopheryl polyethylene
glycol 1000 succinate (Vitamin E-TPGS), Cremophor® EL, Polysorbate 80, and
Pluronic® F85) and polymers (such as poly-(ethyleneoxide)/poly-(propyleneoxide)
block copolymers, and amphiphilic diblock copolymers methoxypolyethylene
glycol-block-polycaprolactone) inhibit P-gp efflux pump. Use of these
ingredients in the formulation can help delivery of sensitive drugs to the eye.
3. Nanoparticles and liposomes: Nanosuspensions of
drugs can be utilized to deliver
poorly soluble drugs, such as flurbiprofen, meth-ylprednisolone acetate, and
glucocorticoids (e.g., hydrocortisone, prednisolone, and dexamethasone) into
the eye. The nanosuspensions can enable enhanced retention at the target site
and sustained-release (SR) properties to the drug. The retention of
nanoparticles in the periocular space versus clearance by blood and lymphatic
circulation would depend on the size and surface properties of the
nanoparticles. Liposomes, lipid vesicles containing an aqueous core, can
protect a drug against enzymatic degradation, increase the capacity to cross
the cell membrane, provide SR, and/or prevent drug efflux.
4. Intraocular implants: Implants can be utilized for drugs
targeted to both the anterior and
posterior segments of the eye for diseases such as proliferative
vitreoretinopathy, CMV retinitis, and endophthalmitis. The implants can be made
with biodegradable or nonbiodegrad-able polymers such as poly(lactic acid)
(PLA), poly(glycolic acid) (PGA), poly(lactide-co-glycolide (PLGA),
poly(glycolide-co-lactide-co-caprolactone (PGLC) copolymer, poly(caprolactone)
(PCL), polyanhydrides, and polyorthoesters (POE). Drugs that have been
investigated for drug delivery by implantable DDS include dexameth-asone,
cyclosporine, 5-fluorouridine (5-FU), triamcilone acetonide, and recombinant
tissue plasminogen activator.
5. Hydrogels: Hydrogels are
three-dimensional, hydrophilic, poly-meric networks capable of absorbing and
holding a large amount of water. Thermosensitive hydrogels prepared by
cross-linking poly(N-isopropylacrylamide) (PNIPAAm) with PEG have been
investigated for drug delivery to the posterior segment of the eye. Drugs such
as bevacizumab and ranibizumab have been tested for delivery in hydrogels.
Related Topics
