Protein Misfolding
| Home | | Biochemistry |Chapter: Biochemistry : Structure of Proteins
Protein folding is a complex process that can sometimes result in improperly folded molecules. These misfolded proteins are usually tagged and degraded within the cell.
PROTEIN MISFOLDING
Protein folding is a
complex process that can sometimes result in improperly folded molecules. These
misfolded proteins are usually tagged and degraded within the cell. However,
this quality control system is not perfect, and intracellular or extracellular
aggregates of misfolded proteins can accumulate, particularly as individuals
age. Deposits of misfolded proteins are associated with a number of diseases.
A. Amyloid diseases
Misfolding of proteins
may occur spontaneously or be caused by a mutation in a particular gene, which
then produces an altered protein. In addition, some apparently normal proteins
can, after abnormal proteolytic cleavage, take on a unique conformational state
that leads to the formation of long, fibrillar protein assemblies consisting of
β-pleated sheets. Accumulation of these insoluble, spontaneously aggregating
proteins, called amyloids, has been implicated in degenerative diseases such as
Parkinson and Huntington and particularly in the age-related neurodegenerative
disorder, Alzheimer disease. The dominant component of the amyloid plaque that
accumulates in Alzheimer disease is amyloid β (Aβ), an extracellular peptide
containing 40–42 amino acid residues. X-ray crystallography and infrared
spectroscopy demonstrate a characteristic β-pleated sheet conformation in
nonbranching fibrils. This peptide, when aggregated in a β-pleated sheet
configuration, is neurotoxic and is the central pathogenic event leading to the
cognitive impairment characteristic of the disease. The Aβ that is deposited in
the brain in Alzheimer disease is derived by enzymic cleavages (by secretases)
from the larger amyloid precursor protein, a single transmembrane protein
expressed on the cell surface in the brain and other tissues (Figure 2.13). The
Aβ peptides aggregate, generating the amyloid that is found in the brain
parenchyma and around blood vessels. Most cases of Alzheimer disease are not
genetically based, although at least 5% of cases are familial. A second biologic
factor involved in the development of Alzheimer disease is the accumulation of
neurofibrillary tangles inside neurons. A key component of these tangled fibers
is an abnormal form (hyperphosphorylated and insoluble) of the tau (τ) protein,
which, in its healthy version, helps in the assembly of the microtubular
structure. The defective τ appears to block the actions of its normal
counterpart.
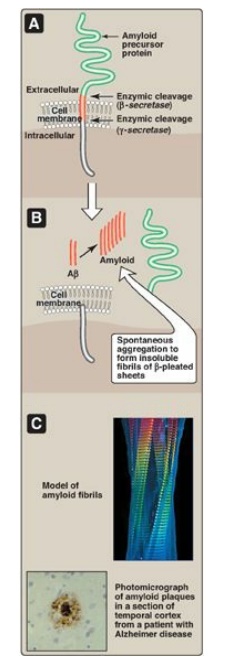
Figure 2.13
Formation of amyloid plaques found in Alzheimer disease (AD). [Note: Mutations
to presenilin, the catalytic subunit of γ-secretase, are the most common cause
of familial AD.]
B. Prion diseases
The prion protein (PrP)
has been strongly implicated as the causative agent of transmissible spongiform
encephalopathies (TSEs), including Creutzfeldt-Jakob disease in humans, scrapie
in sheep, and bovine spongiform encephalopathy in cattle (popularly called “mad
cow” disease). After an extensive series of purification procedures, scientists
were surprised to find that the infectivity of the agent causing scrapie in
sheep was associated with a single protein species that was not complexed with
detectable nucleic acid. This infectious protein is designated PrPSc (Sc =
scrapie). It is highly resistant to proteolytic degradation and tends to form
insoluble aggregates of fibrils, similar to the amyloid found in some other
diseases of the brain. A noninfectious form of PrPC (C = cellular), encoded by
the same gene as the infectious agent, is present in normal mammalian brains on
the surface of neurons and glial cells. Thus, PrPC is a host protein. No
primary structure differences or alternate posttranslational modifications have
been found between the normal and the infectious forms of the protein. The key
to becoming infectious apparently lies in changes in the three-dimensional
conformation of PrPC. It has been observed that a number of α-helices present
in noninfectious PrPC are replaced by β-sheets in the infectious form (Figure
2.14). It is presumably this conformational difference that confers relative
resistance to proteolytic degradation of infectious prions and permits them to
be distinguished from the normal PrPC in infected tissue. The infective agent
is, thus, an altered version of a normal protein, which acts as a “template”
for converting the normal protein to the pathogenic conformation. The TSEs are
invariably fatal, and no treatment is currently available that can alter this
outcome.
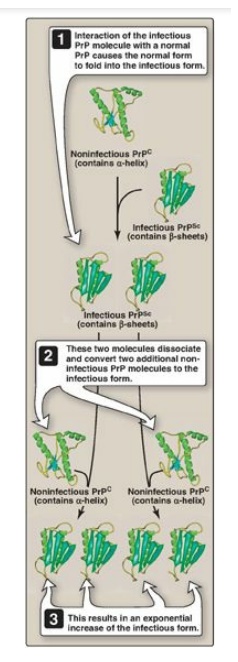
Figure 2.14
One proposed mechanism for multiplication of infectious prion agents. PrP =
prion protein; PrPc = prion protein cellular; PrPSc = prion protein scrapie.
Related Topics
